Figures & data
Figure 1 Case definitions used to identify neuropathic pain conditions in the study sample.
Abbreviations: CLBP-NeP, chronic low back pain with neuropathic pain; HIV-NeP, human immunodeficiency virus-related peripheral neuropathic pain; pDPN, painful diabetic peripheral neuropathy; PTPS-NeP, post-trauma/post-surgical neuropathic pain; SCI-NeP, spinal cord injury with neuropathic pain; SFN, painful peripheral neuropathy with small fiber involvement.
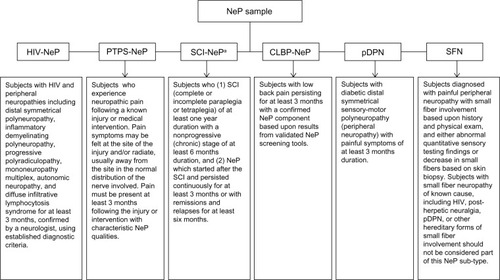
Table 1 Sources used to assign costs to health care resources and lost productivity
Table 2 Neuropathic pain condition samples by pain severity level
Table 3 Demographic and clinical characteristics overall and by degree of severityTable Footnotea
Figure 2 Proportion of subjects prescribed medications to manage neuropathic pain by pain severity level.a
Abbreviations: AED, antiepileptic drug; NSAIDs, nonsteroidal anti-inflammatory drugs; SNRIs, serotonin-norepinephrine reuptake inhibitors; TCAs, tricyclic antidepressants.
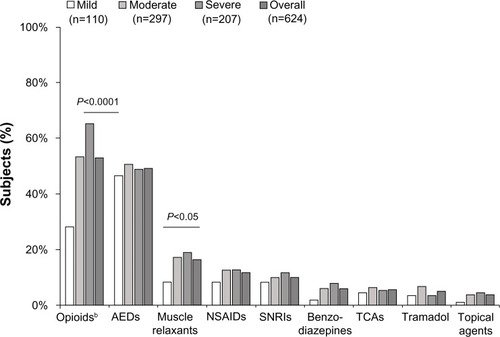
Table 4 Health care resource utilization for neuropathic pain stratified by pain severityTable Footnotea
Figure 3 Impact of neuropathic pain on employment status by pain severity level.
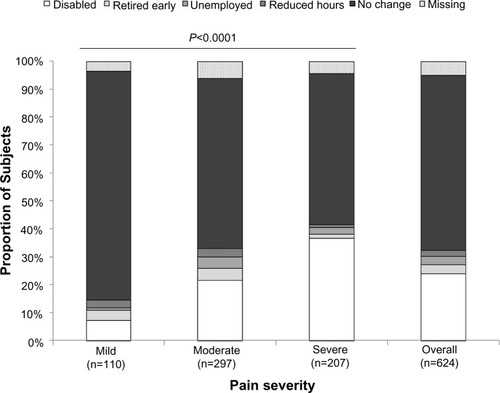
Figure 4 Impact of neuropathic pain on productivity and daily activity evaluated using the WPAI questionnaire, by pain severity level.
Abbreviation: WPAI, Work Productivity and Activity Impairment.
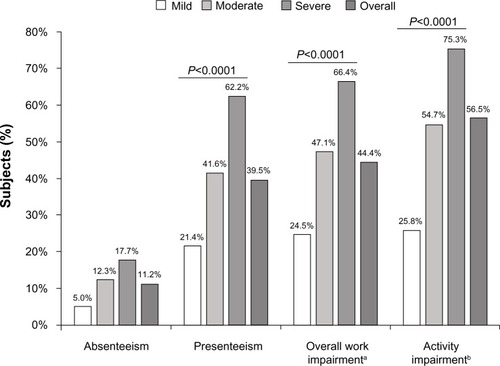
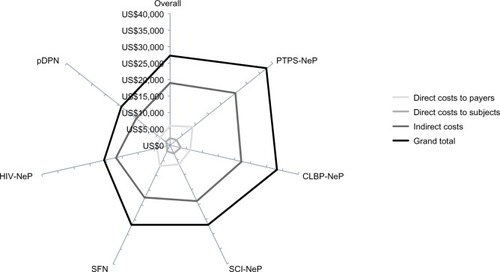
Figure 5 Adjusted least squares mean estimates for annualized costs per subject from multiple linear regression adjusted for confounding demographic and clinical variables.
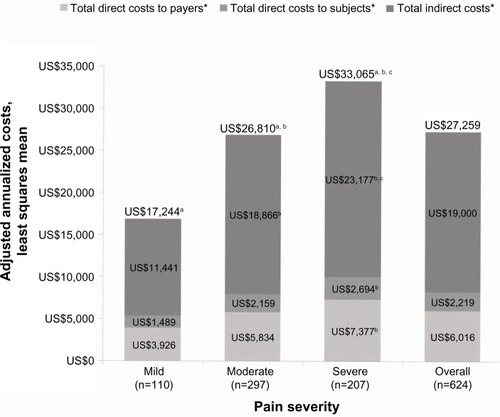
Figure 6 Mean annualized adjusted cost per subject varied by neuropathic pain condition.a
Abbreviations: CLBP-NeP, chronic low back pain with neuropathic pain; HIV-NeP, human immunodeficiency virus-related peripheral neuropathic pain; pDPN, painful diabetic peripheral neuropathy; PTPS-NeP, post-trauma/post-surgical neuropathic pain; SCI-NeP, spinal cord injury with neuropathic pain; SFN, painful peripheral neuropathy with small fiber involvement.