Figures & data
Table 1 General Information and Operative Data of 18 Patients
Figure 1 Preoperative plan and 3D model of the navigation template. (A) The yellow ellipses indicate the CBT screw trajectory planned before the surgery. (B) The navigation template with the segment with the original pedicle screw reconstructed by Mimics. (C and D) The top and back view of the navigation template.
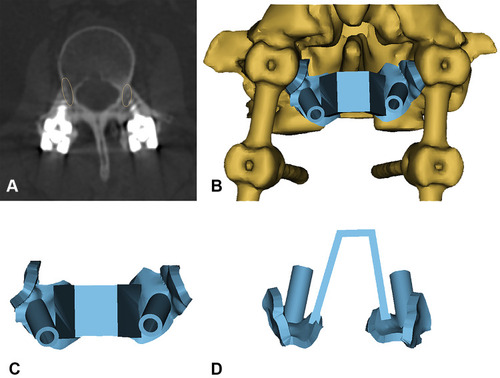
Figure 2 Case 1. A 77-year-old man with ASD of L3-4 underwent revision surgery with CBT screws assisted by a navigation template. (A–D) Preoperative MRI and CT scans revealed L3/4 intervertebral disc herniation and calcification. (E–H) His pre- and postoperative X-ray showed the CBT screws as the fixation method for L3/4.
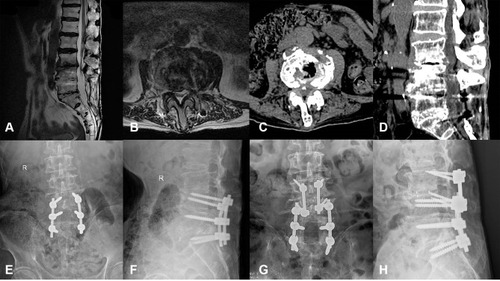
Figure 3 Case 2. A 63-year-old female had undergone L4/5 fusion 5 years prior. She had experienced radiating pain of the left lower limb for half a year and was diagnosed with ASD of L3/4. (A and B) Preoperative X-ray showed the original pedicle screws and cage in L4/5. (C and D) Preoperative CT revealed L3/4 intervertebral disc herniation. (E and F) X-ray after the surgery showed good positioning of the CBT screws.
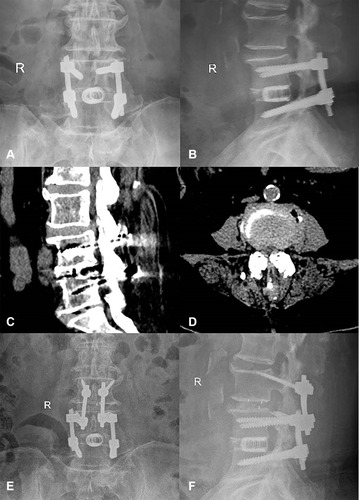
Figure 4 Case 3. A 58-year-old female had undergone prior L5/S1 fusion. She had ASD of L4/5 at the current presentation. (A) Preoperative X-ray showed original fixation of L5/S1. (B) Preoperative MRI revealed a disc herniated into the spinal canal. (C and D) X-ray after the surgery showed good positioning of the CBT screws.
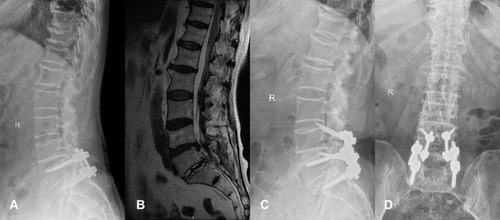
Figure 5 The VAS, ODI, JOA score, and intervertebral height in different assessments. (A) The VAS scores before the operation, 2 weeks after the operation, and at the last follow-up were 6.6±1.2, 3.3±2.0, and 1.6±1.0, respectively; (B) the ODI scores before the operation, 2 weeks after the operation, and at the last follow-up were 43.9±9.4, 24.6±5.1, and 12.8±3.9, respectively; (C) the JOA scores before the operation, 2 weeks after the operation, and at the last follow-up were 14.6±2.9, 20.5±5.1, and 23.8±1.5, respectively. These differences were all statistically significant (P<0.05). (D) The intervertebral heights (mm) before the operation, 2 weeks after the operation, and at the last follow-up were 7.8±2.3, 10.8±1.3, and 10.5±1.4, respectively. There was no significant difference between 2 weeks and the last follow-up (P>0.05).
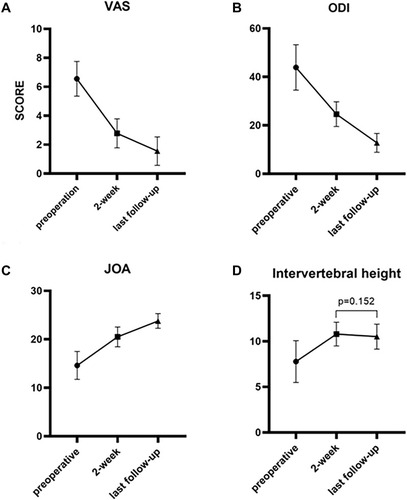
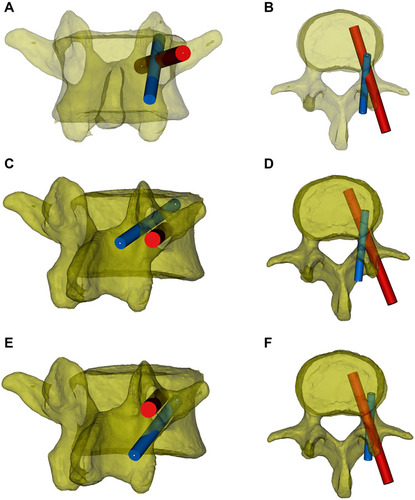
Figure 6 The trajectory relationship between the pedicle screw and CBT screw. The red cylinder represents the pedicle screw, and the blue cylinder represents the CBT screw. (A and B) Using the standard screw placement technique, the trajectories of the pedicle screws and CBT screws partially overlap in the pedicle. (C and D) The original pedicle is close to the inferior wall of the pedicle, and the new CBT screw will course along the superior aspect of the original pedicle screw. (E and F) The original pedicle is close to the superior wall of the pedicle, and the new CBT screw will course under the original pedicle screw.