Figures & data
Table 1 Baseline characteristics for New Zealand residents aged 30–74 years at December 31, 2006 without prior CVD or heart failure hospitalizations
Figure 1 CVD medications dispensed at baseline (July 1, 2006–December 31, 2006) and follow-up (January 1, 2007–December 31, 2011) among 1,766,584 New Zealand residents aged 30–74 years on December 31, 2006 without a history of CVD or heart failure.
Abbreviations: APL, antiplatelet and/or anticoagulant medications; BPL, blood pressure lowering medications; LL, lipid lowering medications; CVD, cardiovascular disease.
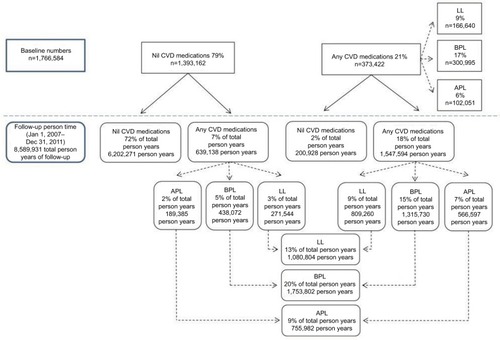
Table 2 CVD medications dispensed during follow-up (January 1, 2007–December 31, 2011) according to baseline dispensing (July 1, 2006–December 31, 2006) among 1,766,584 New Zealand residents aged 30–74 years on December 31, 2006 without prior CVD or heart failure hospitalizations
