Figures & data
Figure 1 (A) Study timelines (analysis and look-back periods) for cohort 1 (national cohort) and cohort 2 (counties of Uppsala and Västerbotten) and (B) patient flow for cohort 1 (national cohort) and cohort 2 (counties of Uppsala and Västerbotten).
Abbreviations: EMR, electronic medical record; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; NPR, National Patient Register.
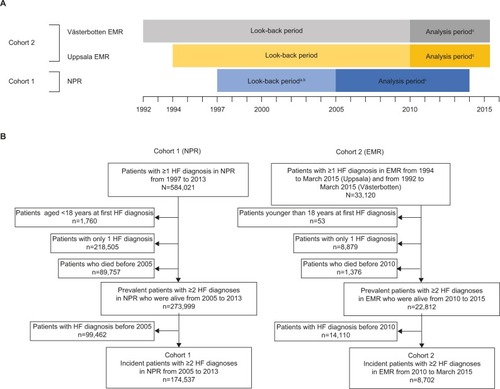
Table 1 Patient demographics and clinical characteristics at baseline for cohort 1 and cohort 2, overall and by HF phenotype (incident patient populations)
Figure 2 Annual incidence per 1,000 inhabitants and prevalence of HF during 2010–2014 in Sweden (cohort 1) and in the counties of Uppsala and Västerbotten (cohort 2).
Abbreviations: EMRs, electronic medical records; HF, heart failure; NPr, National Patient Register.
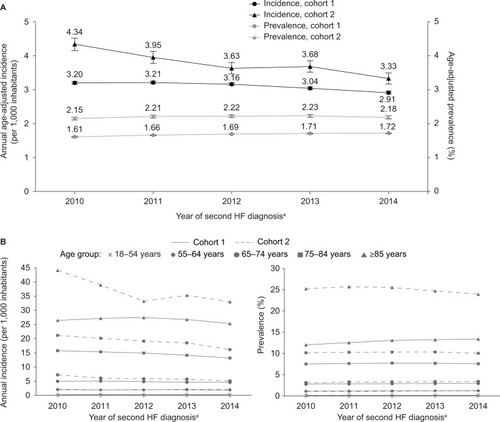
Table 2 Key laboratory measures at baseline for cohort 2, overall and by HF phenotype (incident patient population)
Figure 3 Diagnostic work-up of patients in cohort 2 in the 6 months before and after the year of first HF diagnosis: (A) by index year and (B) according to setting of HF diagnosis.
Abbreviations: Echo, echocardiography; HF, heart failure; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
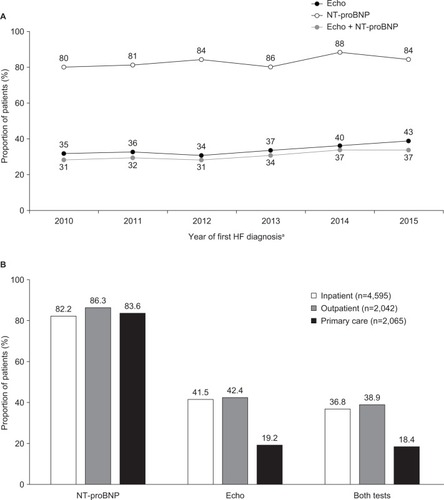
Table 3 COX and Fine and Gray regression analyses of 1-year all-cause and CVD-related mortality with Kaplan–Meier and cumulative incidence function estimates for 1-year mortality (cohort 1, incident HF population)
Figure 4 Trends in the most common causes of death for the prevalent HF population (cohort 1) between 2005 and 2013.
Abbreviations: AF, atrial fibrillation; HF, heart failure; IHD, ischemic heart disease; MI, myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction.
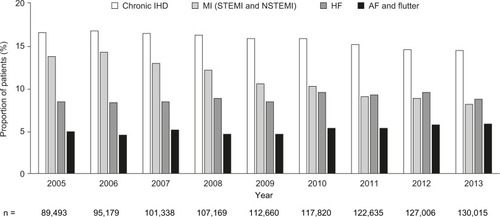
Table 4 COX and Fine and Gray regression analyses of 1-year all-cause and CVD-related mortality with Kaplan–Meier and cumulative incidence function estimates for 1-year mortality (cohort 2, incident HF population)
Data availability
Major findings from the study will be published in scientific manuscripts only. The data will not be made available in any other format in order to preserve the privacy of the patients in compliance with local laws and regulation.
