Figures & data
Table 1 Characteristics of Included Studies
Figure 2 Graphical presentation of quality assessment of 19 studies included in the systematic review (QUIPS risk of bias assessment).
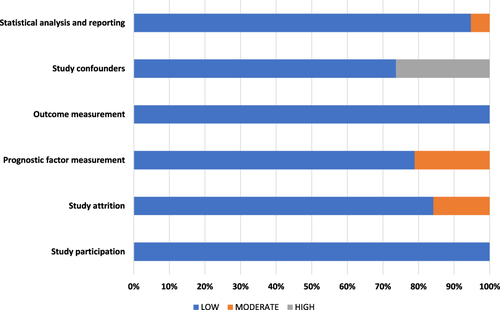
Figure 3 Meta-analysis of studies on the association between post-operative C-reactive protein with overall survival (A), CRC-specific survival (B) and recurrence-free survival (C) among patients with colorectal cancer. (A): Hazard ratio of CRP on overall survival; N/events = 3174/1033. (B): Hazard ratio of CRP on CRC-specific survival; N/events = 1850/352. (C): Hazard ratio of CRP on recurrence-free survival; N/events = 1177/228.
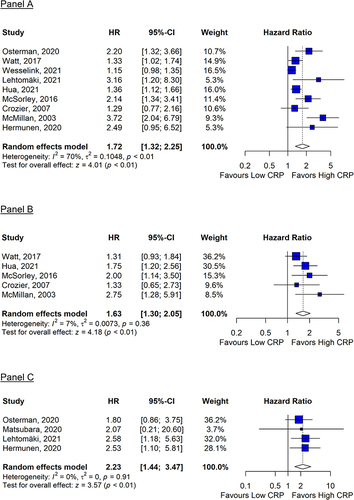
Figure 4 Sensitivity meta-analysis of studies on the association between post-operative C-reactive protein with overall survival (A–C) and CRC-specific survival (D and E) among patients with colorectal cancer. (A): Hazard ratio of overall survival predicted by CRP (cut-off = 10mg/L) assessed ≥4 weeks post-operatively; N/events = 1190/428. (B): Hazard ratio of overall survival predicted by CRP (cut-off = 10mg/L) assessed ≥4 weeks post-operatively for studies that controlled for age and cancer stage; N/events = 710/275. (C): Hazard ratio of overall survival predicted by CRP (cut-off range = 150–170mg/L) assessed ≤1 week post-operatively; N/events = 1270/478. (D): Hazard ratio of CRC-specific survival predicted by CRP (cut-off = 10mg/L) assessed ≥4 weeks post-operatively for studies that controlled for age and cancer stage; N/events = 480/94. (E): Hazard ratio of CRC-specific survival predicted by CRP (cut-off range = 150–170mg/L) assessed ≤1 week post-operatively; N/events = 1776/340.
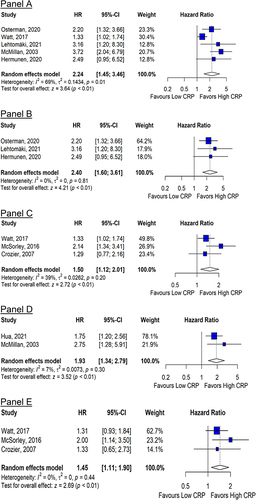
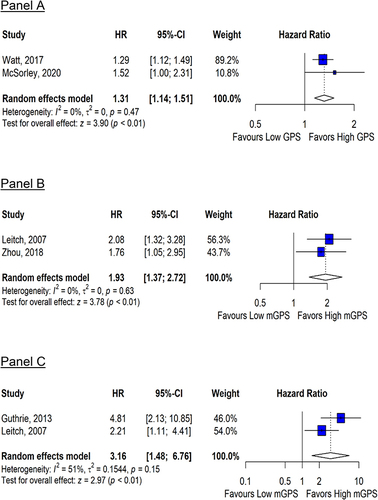
Figure 5 Meta-analysis of studies on the association of the Glasgow Prognostic Score with overall survival (A), and the modified Glasgow Prognostic Score with overall survival (B) and cancer-specific survival (C) among patients with colorectal cancer. (A): Hazard ratio of overall survival per unit increase in GPS assessed ≤1 week post-operatively; N/events = 1357/408. (B): Hazard ratio of overall survival per unit increase in mGPS assessed ≥4 weeks post-operatively; N/events = 665/126. (C): Hazard ratio of cancer specific survival per unit increase in mGPS assessed ≥4 weeks post-operatively; N/events = 355/49.