Figures & data
Figure 1 Scheme of defining group indicating immediate surgery group of ideal or appropriate candidates for AS and delayed surgery imitating group of ideal or appropriate candidates for AS except accompanying with clinically apparent LNM.
Abbreviations: AS, active surveillance; CCND, central compartment neck node dissection; ETE, extrathyroidal extension; LNM, lymph node metastasis; MRND, modified radical neck dissection; PTMC, papillary thyroid microcarcinoma; TT, total thyroidectomy.
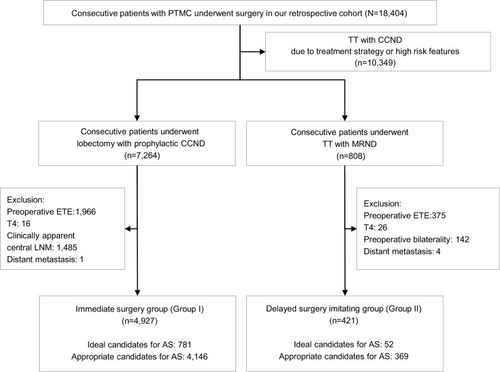
Figure 2 Flow chart presenting the oncologic outcomes of immediate surgery group and delayed surgery imitating group with low-risk PTMC potentially eligible for AS.
Abbreviations: AS, active surveillance; CCND, central compartment neck node dissection; MRND, modified radical neck dissection; PTMC, papillary thyroid microcarcinoma; TT, total thyroidectomy.
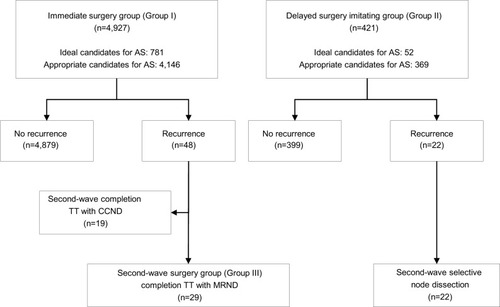
Table 1 Comparison of clinicopathological characteristics between patients with low-risk PTMC without LNM who underwent lobectomy with prophylactic CCND (N=4,927) (Group I) and patients with low-risk PTMC except clinically apparent LNM who underwent total thyroidectomy with MRND (N=421) (Group II)
Figure 3 Comparison of disease-free survival according to patients’ Group.
Notes: (A) Comparison of disease-free survival of patients with low-risk PTMC who underwent lobectomy with prophylactic central cervical node dissection (Group I) with that of patients with low-risk PTMC except clinically apparent lymph node metastasis who underwent total thyroidectomy with modified radical neck dissection (Group II). (B) Comparison of disease-free survival of patients with second-wave surgery due to lateral LN recurrence (Group III, subgroup of Group I) with that of Group II. P-value was determined by the log-rank test.
Abbreviation: PTMC, papillary thyroid microcarcinoma.
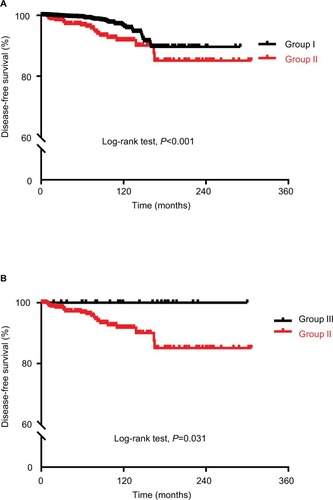
Table 2 Comparison of clinicopathological characteristics in patients with low-risk PTMC who underwent second-wave MRND following initial immediate surgery (N=29) (Group III) and patients with low-risk PTMC except clinically apparent LNM who underwent total thyroidectomy with MRND (N=421) (Group II)
