Figures & data
Table 1 Patients’ characteristics
Figure 1 Each separate radiographic image and the 3DMMI of a 16-year-old boy with osteosarcoma with massive involvement.
Notes: (A) Plain film showing osteogenic lesion of the right ilium and periacetabulum. (B) 3D-CT images combined with contrast-enhanced CTA. (C) Contrast-enhanced MRI showing large soft tissue mass in the pelvis. (D) Contrast-enhanced MRN showing the sacral nerves and the tumor. (E) Anterolateral view of 3DMMI showing the tumor extended from periacetabulum to kidney level with involvement of the sacrum. Although pushed medially, the right external iliac vessels and ureter were free from the tumor due to the protection of the iliacus muscle and psoas major muscle. (F) Posterior and transverse plane of 3DMMI. Massive sacrum bone edema was noted. The right second and third sacral nerves (DCN) were discontinued, while the left were intact, which might indicate involvement of the nerves. This information was very useful for accurate preoperative planning. PSI were also designed to help the resection, according to the virtual surgical planning.
Abbreviations: 3DMMI, 3D-multimodality image; A, artery; Ba, bladder; Bo, bone, translucent; CP, cutting plane; CTA, computed tomography angiography; DCN, discontinued nerves; Ed, edema, translucent, considered to be bone invasion; Ki, kidney; M, muscle, translucent; MRN, magnetic resonance neurography; MRI, magnetic resonance imaging; N, nerve; Pr, prostate; PSI, patient-specific instrument; Tu, tumor; Ur, ureter; V, vein.
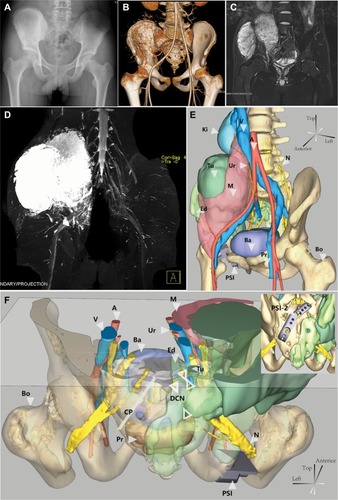
Figure 2 3DMMI-based 3D-printed PSI helped achieve precise resection.
Notes: (A) Intraoperative photo showing osteotomy with PSI. (B) A 3D-printed pelvic model, derived from the 3D-multimodality images, providing intraoperative visual and haptic perception of the surgery. (C) The resected specimen was in high conformity with the simulated surgery, both with 3D-multimodality image-based PSI.
Abbreviations: 3DMMI, 3D-multimodality images; PSI, patient-specific instruments;
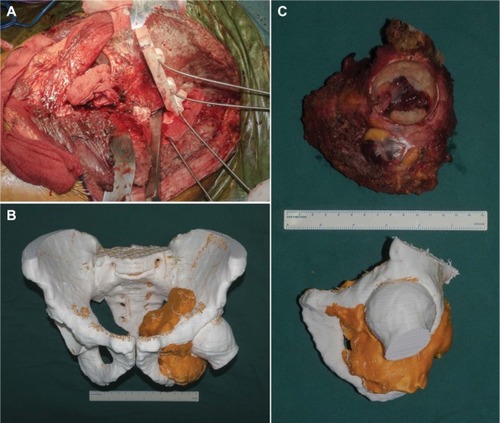
Figure 3 3D-multimodality image-based virtual surgical planning and 3D-printed PSI helped the reconstruction of the pelvis after tumor resection.
Notes: (A) An intraoperative photo showing PSI-guided preparation of FH graft, which was used later to fill the gaps between the prosthesis and the ilium. The PSI-1 also facilitated the screw fixation by predrilling holes in the FH graft, combined with PSI-2 in (B). (B) 3D-multimodality image-based virtual surgical planning showing the reconstruction with PSI-2 and the worked FH. PSI-2 was also used to indicate the simulated proper rotation center of the FH. The picture in the left bottom illustrating the gap, between the prosthesis and the ilium, was filled by the FH graft suitably. (C–E) Intraoperative photos and postoperative plain film showing satisfactory reproduction of the virtual surgical planning.
Abbreviations: A, artery; Ba, bladder; FH, femoral head; N, nerve; Pro, prosthesis; Pr, prostate; PSI, patient-specific instruments; Ur, ureter; V, vein.
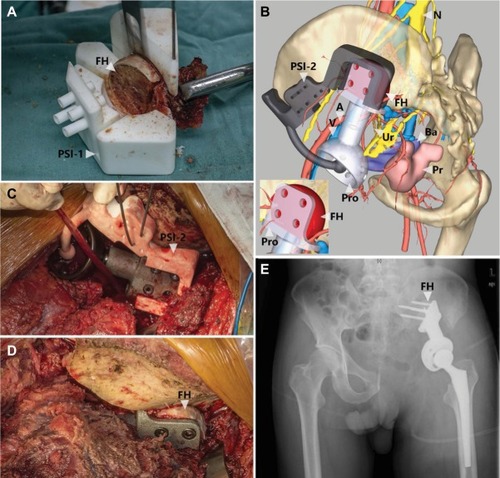
Table 2 Intraoperative issues and early outcome
