Figures & data
Figure 1 (A) High-tie, the IMA is ligated at its origin within 1 cm from the aorta, with dissection of the apical lymph nodes (LN); (B) Low-tie, the IMA and the proximal left colic artery (LCA) are skeletonized, LCA is preserved, the superior rectal artery (SRA) is ligated, LN dissection medially along the IMA root, including the abdominal aortic (AA) plane.
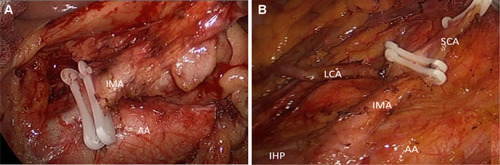
Figure 2 (A) Tension-free anastomosis after low-tie of IMA and preservation of LCA; (B) Completion of laparoscopic surgery for rectal cancer and skin closure of ports; (C-D) Retrieved specimen after low-tie and total mesorectal excision (TME) for rectal cancer.
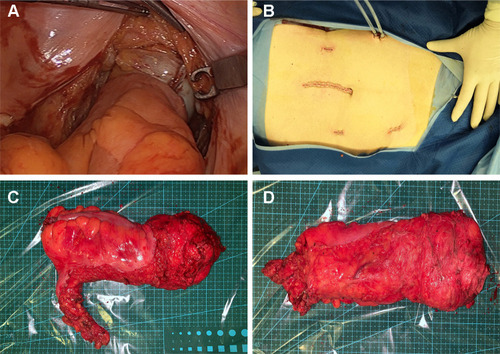
Table 1 Clinicodemographic Profile of Patients with Low-Tie vs High-Tie of the Inferior Mesenteric Artery in Laparoscopic Anterior Resection of Rectal Cancer, N=614
Table 2 Operative Findings of Rectal Cancer Patients with LT vs HT in Laparoscopic Anterior Resection of Rectal Cancer, N=614
Table 3 Risk Factors for Anastomotic Leakage in Patients with LT vs HT in Laparoscopic Anterior Resection for Rectal Cancer, N=614
Table 4 Hazard Ratio in for Anastomotic Leakage in Patients with LT vs HT in Laparoscopic Anterior Resection for Rectal Cancer, N=614
Table 5 Long-Term Results of Overall Survival (OS) and Disease-Free Survival (DFS) in Patients with LT vs HT Anterior Resection of Rectal Cancer, N=614
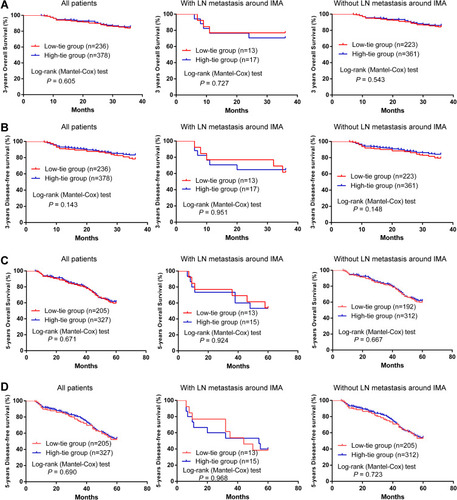
Figure 3 Long-term outcomes in the low-tie groups and high-tie groups. (A) 3-years OS with all patients, LN metastasis around IMA patients, and without LN metastasis around IMA patients; (B) 3-years DFS with all patients, LN metastasis around IMA patients, and without LN metastasis around IMA patients; (C) 5-years OS with all patients, LN metastasis around IMA patients, and without LN metastasis around IMA patients; (D) 5-years DFS with all patients, LN metastasis around IMA patients, and without LN metastasis around IMA patients.