Figures & data
Figure 1 Localization of extracranial MRT (EU-RHAB registry data). (A) Anatomical localization of patients with extracranial MRT (n=185) registered between 2007 and 2020. The most common localizations of primary tumors are highlighted bold. (B) Distribution of patients with extracranial MRT (n=185) by age and localization registered between 2004 and 2020. * Patients with ATRT and RTK or eMRT. (C) Distribution of patients with eMRT (n=118) by age and primary site registered between 2004 and 2020. *Other sites: bladder (n=2), heart (n=1), skin (n=2), pancreas (n=1), adrenal gland (n=1), clavicle (n=1), brachial plexus (n=1).
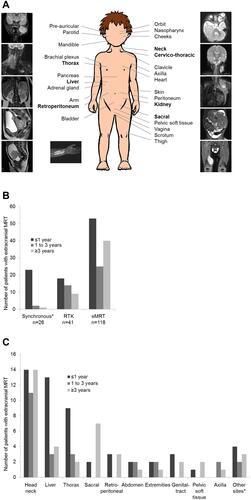
Figure 2 Overview of molecular features of the different extracranial MRT subgroups (based on Chun et alCitation23 and Andrianteranagna et alCitation28).
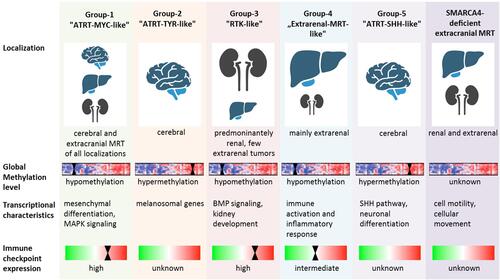
Table 1 Summary of Retrospective and Prospective Trials/Registries of Extracranial MRT
Figure 3 Response to standardized chemotherapy in a patient with extensive primary eMRT – Imaging results. (A) Diagnostic imaging at 27 months of age with inoperable, abdominal eMRT (14x14x9.8 cm), without distant metastasis, without germline mutation. (B) MRI before confirmed pathological diagnosis of eMRT, one course I2-VAd (ifosfamide, vincristine, Adriamycin) according CWS VAIA protocol, and after confirmed diagnosis, two courses ICE (ifosfamide, cyclophosphamide, etoposide) according EU-RHAB were given. After three courses of chemotherapy, tumor regression (5.6x8.8x4.2 cm), and stable disease < 25% was detected. (C) Imaging following chemotherapy according EU-RHAB was continued with one course of DOX (doxorubicin) and VCA (vincristine, cyclophosphamide, actinomycin D). Eventually the tumor was resected subtotally, and stable disease < 10% was achieved. (D) Following resection radiotherapy of the tumor bed (for abdomen up to 36 Gy) with boost to celiac trunk (up to 45 Gy) was performed, and therapy was completed with one course of VCA (vincristine, cyclophosphamide, actinomycin D), IC (ifosfamide, cyclophosphamide), VC (vincristine, cyclophosphamide) and DOX (doxorubicin) was given. The patient achieved complete remission, and is alive at 32 months following diagnosis.
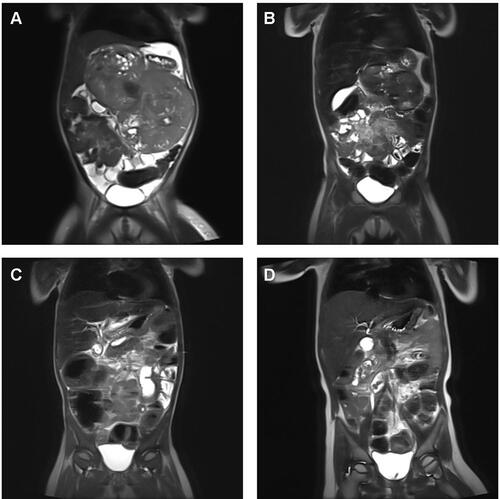
Table 2 Overview of Preclinical Studies on Pediatric MRT
Figure 4 Overview of immunotherapy in pediatric MRT.
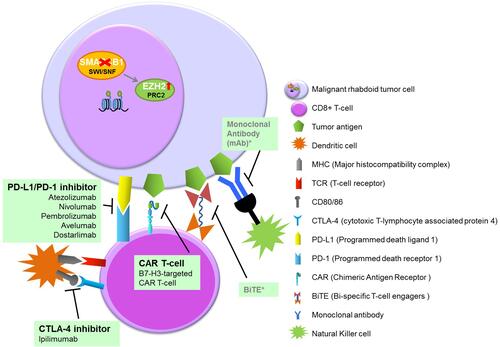
Table 3 Overview of Ongoing Experimental Clinical Trials in Pediatric Extracranial MRT
