Figures & data
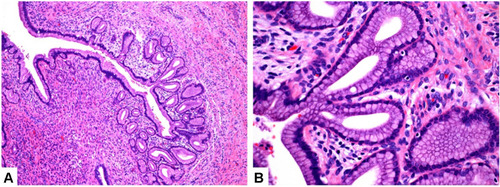
Figure 1 Colposcopy image. (A) After placing the speculum, the appearance of the cervix; (B) After magnification of the cervical colposcopy image, clear watery secretions covering the cervix can be seen; (C) The appearance of the cervix after the secretion is wiped off with a cotton swab (D–F). A lot of large gland openings can be observed on the surface of the cervix, and the gland opening is continuously secreting huge amount of watery secretions. (G) Abnormal blood vessels on the surface of the cervix can be observed. (H and I) Colposcopy image of the cervix after using Lugol’s iodine.
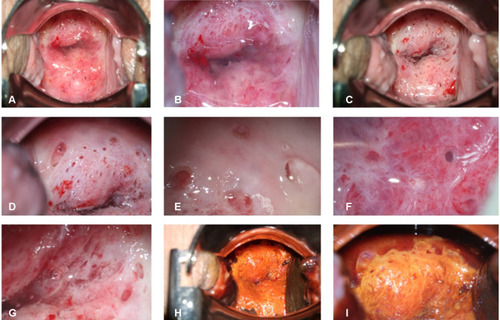
Figure 2 Histopathology of LEEP specimen. HE staining of minimal deviation adenocarcinoma and loss of lobular structure with invasive growth. (A) Tumorous glands are diffusely distributed and infiltrate extensively, and cancerous involvement can be seen on the cervical intimal margin (upper border). (B) The glands are well differentiated, similar to the gastric glands. (C) Fibrous reaction and chronic inflammatory cell infiltration can be seen around the gland.
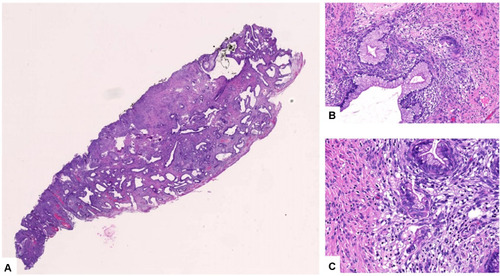
Figure 3 MRI image of the patient. The uterus presents posterior flexion, and the size of the uterus is 5.4cm × 6.0cm × 4.5cm. The endometrium is not thickened, without obvious abnormal signal. The cervix has a mass shadow, the size is about 3.6cm × 3.4cm × 4.4cm, T1WI showed iso-low signal (A and B), T2WI showed a little high signal (C and D), DWI showed high signal, uneven enhancement was seen after enhancement, and no obvious abnormal signal foci were seen around the uterus. There were no obvious abnormalities in bilateral ovaries and bilateral appendage areas. The bladder is well filled, the bladder wall is not thickened, and there is no obvious abnormal signal shadow on the bladder wall. There was no obvious abnormal signal shadow in the vagina, urethra and rectum, and there was a slight swollen lymph node shadow beside the right iliac blood vessel. A small amount of free fluid signal in recto-uterine pouch.
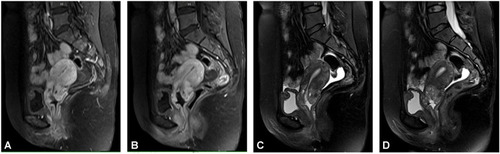
Figure 4 Lobular endocervical glandular hyperplasia (LEGH). Lobular endocervical glandular hyperplasia (LEGH) is also called cervical gland phyllodes hyperplasia. The phyllodes hyperplasia is generally located on the upper half of the cervical epithelium, and the glands are well differentiated. At a smaller magnification, the nuclei gather at the base like a necklace. ((A), magnified ten times) Gastric type differentiated glands, no fibrous reaction and inflammatory cell infiltration ((B), magnified forty times).