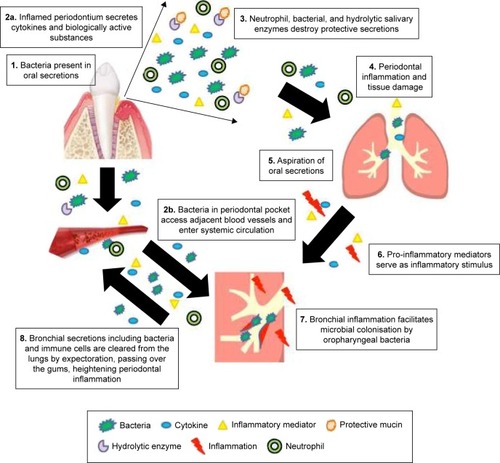
Notes: (
1) Periodontal bacteria are found in oral secretions and could result in systemic inflammation by two mechanisms. (
2a) Inflammation of the periodontium causes production of local cytokines and other biologically active molecules that enter the systemic circulation by diffusion. These activate both the endothelium and circulating immune cells, which contribute to the inflammatory burden by the release of activating and destructive mediators. This process also occurs in the lungs, causing pulmonary inflammation. (
3) Protective secretions and mucins are destroyed by neutrophils and hydrolytic salivary enzymes produced by bacteria. (
4) Unresolved periodontal inflammation results in damage to periodontal tissue and alveolar bone. (
5) Cytokines, bacteria, neutrophils, and other biologically activated mediators are aspirated into the respiratory tree and initiate bronchial inflammation perpetuated by upregulation of the expression of adhesion receptors on mucosal surfaces. (
6) Pro-inflammatory mediators serve as an additional inflammatory stimulus and induce a more active response in the lungs.
Citation99 (
7) Bronchial inflammation facilitates microbial colonization by oropharyngeal bacteria
Citation39,Citation98,Citation107,Citation112,Citation113 and local tissue destruction.
Citation67 (
8) Infected and inflamed bronchial secretions increase the inflammatory load in the periodontium following expectoration. An alternative mechanism is represented in (
2b). Periodontal pathogens enter gingival vasculature through micro-ulcerations in the epithelium allowing hematogenous dissemination of inflammatory mediators and bacteria.
Citation40 This bypasses stages 3–6 and has a resultant influence at stage 7.