Figures & data
Figure 1 Patient selection.
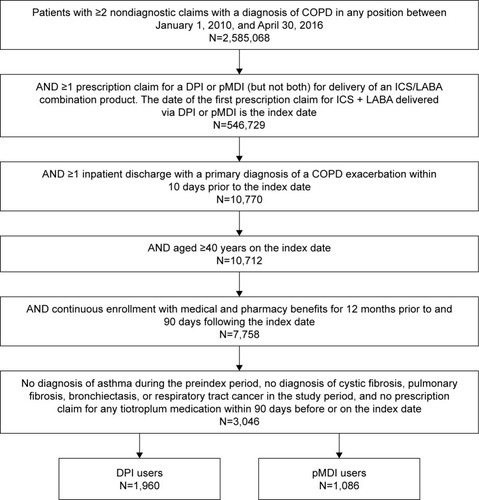
Table 1 Demographic and clinical characteristics
Table 2 Health care resource utilization and costs in the 12-month preindex period
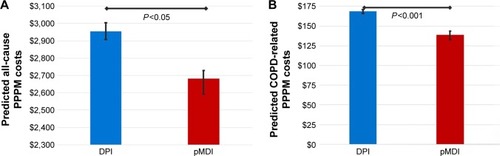
Table 3 All-cause and COPD-related HRU and costs in the 90-day postindex period
Figure 2 Kaplan–Meier curves comparing time (in days) from index date to first (A) all-cause readmission and (B) AECOPD-related readmission within 60 days postdischarge for DPI and pMDI cohorts.
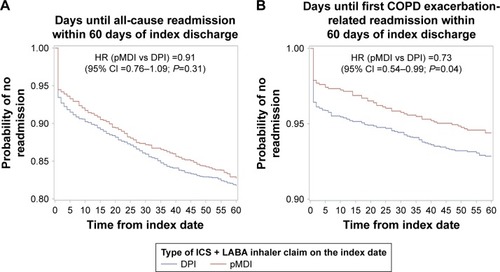
Table 4 All-cause and AECOPD readmissions