Figures & data
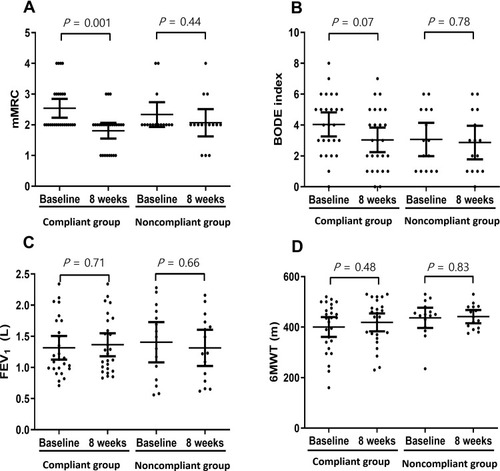
Figure 1 Study design for unsupervised home-based pulmonary rehabilitation. Baseline measurements were obtained after enrolling eligible patients. The patients performed unsupervised home-based pulmonary rehabilitation after receiving 1-h education on it at baseline. The patients were called weekly and encouraged to achieve home-based pulmonary rehabilitation and maintain diaries of recordings. After 8 weeks, patients were categorized as either the compliant or noncompliant group, and measurements were analyzed for outcomes.
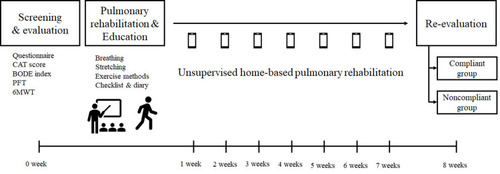
Table 1 Baseline Characteristics
Figure 2 Study flow chart of the enrollment of patients with COPD for the unsupervised home-based pulmonary rehabilitation study. A total of 50 patients were screened for the study; of them, 9 patients were excluded. Among the enrolled 41 patients, 26 patients were grouped as compliant and 15 as noncompliant, based on adherence and nonadherence to 30-min exercise per day for at least 3 days per week, respectively.
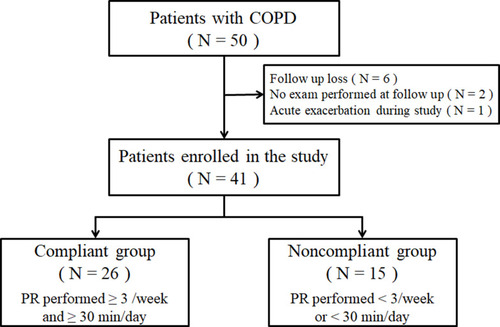
Table 2 Changes in Clinical, Spirometry, and 6-Min Walking Test Outcomes from Baseline to 8 Weeks in Both Groups
Figure 3 Primary outcome and CAT changes after 8 weeks of home-based pulmonary rehabilitation. A scatter plot representing chronic obstructive pulmonary disease (COPD) assessment test (CAT) results at baseline and 8 weeks. The plot is presented as mean with 95% confidence interval (CI). The differences between baseline values and values obtained after 8 weeks were analyzed using an independent two-sample t-test. In the compliant group, CAT scores significantly improved (16.46 ± 7.80 vs 11.85 ± 7.23; P = 0.03), whereas in the noncompliant group, there was no significant change in CAT scores (16.53 ± 7.38 vs 18.93 ± 10.59; P = 0.48).
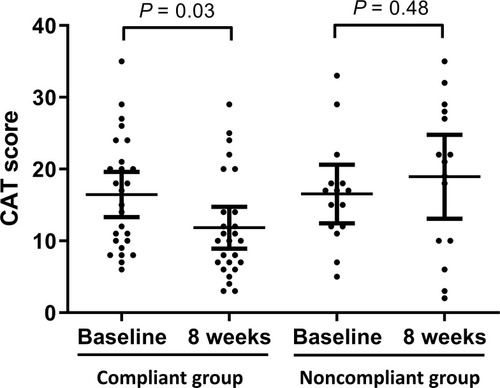
Figure 4 Secondary outcome measurements after 8 weeks of home-based pulmonary rehabilitation obtained for mMRC, BODE index, FEV1, and 6MWT. The scatter plot presents baseline and 8 weeks outcomes. The plots are presented as mean with 95% confidence interval. Differences between the baseline values and values obtained after 8 weeks were analyzed using an independent two-sample t-test. In the compliant group, mMRC scores (2.54 ± 0.76 vs 1.81 ± 0.63; P = 0.001, (A)) significantly improved after 8 weeks. However, the BODE index (4.04 ± 1.93 vs 3.04 ± 1.97; P = 0.07, (B)), FEV1 (1.32 ± 0.47 vs 1.37 ± 0.46; P = 0.71, (C)), and 6MWT results (400.35 ± 97.31 vs 418.58 ± 88.07; P = 0.48, (D)) did not show significant changes. In the noncompliant group, mMRC scores (2.33 ± 0.72 vs 2.07 ± 0.80; P = 0.44, (A)), BODE index (3.07 ± 1.94 vs 2.87 ± 1.96; P = 0.78, (B)), FEV1 (1.41 ± 0.58 vs 1.31 ± 0.52; P = 0.66, (C)), and 6MWT results (436.67 ± 72.03 vs 441.53 ± 47.20; P = 0.83, (D)) were not significantly different.