Figures & data
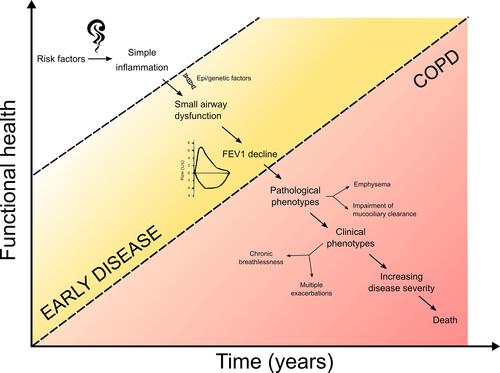
Figure 1 Hypothetical trajectories of lung function (adjusted especially for age but also sex, height and race) that may be seen in the general population of smokers. Horizontal colored areas defined by the vertical axis represent COPD severity according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) staging. Trajectory 1 refers to the lung function trajectory of smokers with decline due to age alone. He/she may not experience any respiratory symptoms or develop COPD. Trajectory 2 represents smokers who have mild decline greater than age-related changes. He/she may eventually cross the COPD diagnostic threshold but may only develop mild disease or respiratory symptoms. Trajectory 3 represents a smoker with an even greater lung function decline and will develop more severe COPD in later life with the associated high morbidity burden. The “early disease” process (represented by the shaded rectangle) is rarely identified and yet should contain the initiating clues to development of COPD especially in those with a more active disease process.
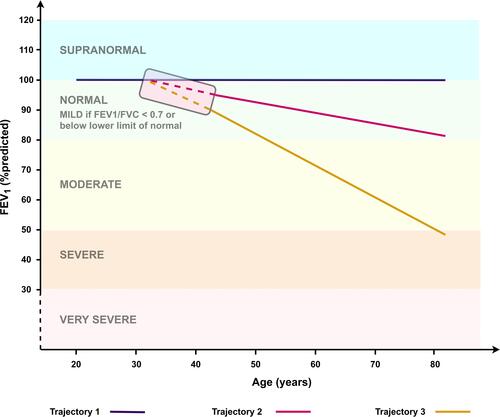
Figure 2 Non-proportional Venn diagram of COPD. This diagram illustrates the subsets of patients with chronic bronchitis, emphysema and asthma. The red areas (subsets 1–7) consist of COPD patients with differing clinical and pathological phenotypes of COPD. The majority of patients with COPD will have airflow obstruction together with features of chronic bronchitis and emphysema (subset 1). Some COPD patients may predominantly have symptoms of chronic bronchitis (subset 2) or emphysema (subset 3) or even have features of asthma (subsets 5–7). Those without airflow obstruction (subsets 8–10) are not classified as having COPD but may have pathophysiological features such as chronic bronchitis (subset 8), emphysema (subset 10) or both (subset 9) that if detected and treated early may prevent progression to established COPD. Adapted with permission of the American Thoracic Society. Copyright © 2021 American Thoracic Society. All rights reserved. American Thoracic Society. Definitions, epidemiology, pathophysiology, diagnosis, and staging. Am J Respir Crit Care Med. 1995;152(5pt2):S78–S83. The American Journal of Respiratory and Critical Care Medicine is an official journal of the American Thoracic Society. Readers are encouraged to read the entire article for the correct context at https://www.atsjournals.org/doi/10.1164/ajrccm/152.5_Pt_2.S78. The authors, editors, and The American Thoracic Society are not responsible for errors or omissions in adaptations.Citation13
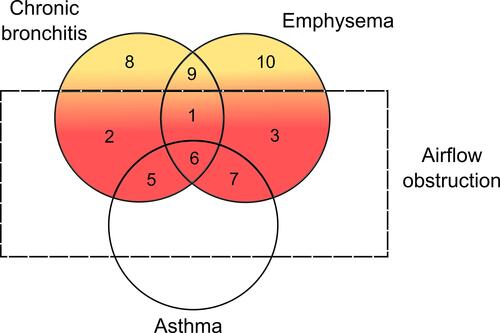
Table 1 Studies of Commonly Researched Blood Biomarkers in COPD with Cohort Demographic Features and Associated Clinical/Physiological Status Together with Outcomes Where These Have Been Documented
Figure 3 Hypothetical timeline of disease progression in susceptible smokers. Subjects who are persistently exposed to risk factors (eg, cigarette smoke, air pollutants, biomass fuel smoke) suffer from low-grade airway inflammation. However, a subset of them (which may be genetically determined or dependent on epigenetic factors) are predisposed to develop COPD in later life over many years. These subjects may initially develop small airway dysfunction and if highly active, will have rapid lung function decline until they cross the diagnostic threshold for COPD. Many COPD patients are diagnosed only when they suffer from established symptoms and impaired health. At this point, the complexities of the pathological and clinical phenotypes are already established and damage is irreversible which increases the challenge of developing disease-modifying therapies for clinical trials. The most logical approach is to identify disease earlier when the pathological inflammation is only influenced by risk factors and gene/environment susceptibility (white to yellow zone) and not by amplification due to tissue damage and progression to variable phenotypes and their combinations (red zone).