Figures & data
Table 1 Characteristics of Studies Observing Relapse Events Following an Exacerbation
Table 2 Characteristics of Studies Observing Recurrence or Re-Exacerbation Events Following an Exacerbation
Table 3 Characteristics of Studies Observing Treatment Failure Following an Exacerbation
Table 4 Characteristics of Studies Observing Non-Recovery or Time to Recovery Events Following an Exacerbation
Figure 1 PRISMA* flow diagram of included and excluded articles. *Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71.Citation26
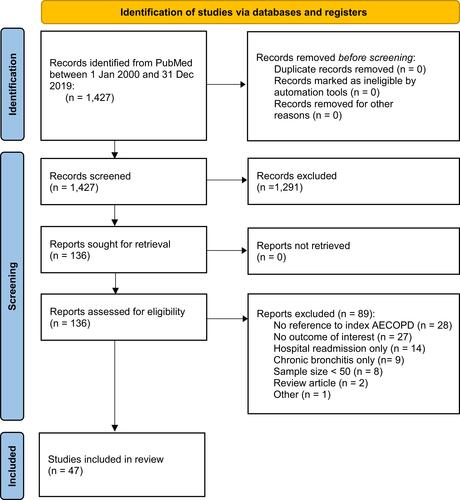
Table 5 Summary of the Four Terms Identified to Describe Subsequent AECOPD Events
Figure 2 Reported proportions of patients with (A) relapse event, (B) recurrence/re-exacerbation event, (C) treatment/clinical failure, and (D) non-recovery, by starting point of observation time frame. (A) Includes estimates from 12 observational studies reporting outcomes using a relapse term and definition. Defined as a re-visit to the emergency department or physician for a worsening of symptoms but typically not differentiated from “recurrence” or “re-exacerbation”. One study used two definitions for relapse at 14 days and thus has two data points. Domenach (2013) is not plotted because the study did not report a timeframe. (B) Includes estimates from 10 observational studies reporting outcomes using a recurrence/re-exacerbation term and definition. Mostly defined as a “re-exacerbation” (n = 3), a prescription course of corticosteroids or antibiotics (n = 3), or as a composite outcome (n = 3) including death or AECOPD treatment and/or remission. Some studies (n = 4) required recovery of initial AECOPD prior to subsequent AECOPD. Two studies have data points at several time horizons (30, 90, 180, and 365 days from Wang et al [2012] and 30, 60, 90, and 180 days from Johannesdottir et al [2013]). Bartziokas et al (2014) reported proportion at 3 months and 6 months in “low uric acid” and “high uric acid” groups, but not overall, and therefore these data points are not presented in the figure. (C) Includes estimates from 12 observational studies reporting outcomes using a treatment failure term and definition with some definitions similar to relapse and non-recovery. Often included death (n = 7) and/or was related to in-hospital treatment failure (n = 6). (D) Includes estimates from seven observational studies reporting outcomes using a non-recovery term and definition. Some studies (n = 2) reported estimates at multiple time points and using different methods of measurement (eg, non-recovery ascertained daily symptom score reports or spirometry). Most were from the London COPD cohort. Two studies have multiple data points due to different measurement methods (symptom report and peak expiratory flow, Donaldson [2015] and Seemungal [2000]) over several time horizons (Seemungal [2000] at 35 days and 91 days).Abbreviations: AECOPD, acute exacerbation of chronic obstructive pulmonary disease; ED, emergency department.
![Figure 2 Reported proportions of patients with (A) relapse event, (B) recurrence/re-exacerbation event, (C) treatment/clinical failure, and (D) non-recovery, by starting point of observation time frame. (A) Includes estimates from 12 observational studies reporting outcomes using a relapse term and definition. Defined as a re-visit to the emergency department or physician for a worsening of symptoms but typically not differentiated from “recurrence” or “re-exacerbation”. One study used two definitions for relapse at 14 days and thus has two data points. Domenach (2013) is not plotted because the study did not report a timeframe. (B) Includes estimates from 10 observational studies reporting outcomes using a recurrence/re-exacerbation term and definition. Mostly defined as a “re-exacerbation” (n = 3), a prescription course of corticosteroids or antibiotics (n = 3), or as a composite outcome (n = 3) including death or AECOPD treatment and/or remission. Some studies (n = 4) required recovery of initial AECOPD prior to subsequent AECOPD. Two studies have data points at several time horizons (30, 90, 180, and 365 days from Wang et al [2012] and 30, 60, 90, and 180 days from Johannesdottir et al [2013]). Bartziokas et al (2014) reported proportion at 3 months and 6 months in “low uric acid” and “high uric acid” groups, but not overall, and therefore these data points are not presented in the figure. (C) Includes estimates from 12 observational studies reporting outcomes using a treatment failure term and definition with some definitions similar to relapse and non-recovery. Often included death (n = 7) and/or was related to in-hospital treatment failure (n = 6). (D) Includes estimates from seven observational studies reporting outcomes using a non-recovery term and definition. Some studies (n = 2) reported estimates at multiple time points and using different methods of measurement (eg, non-recovery ascertained daily symptom score reports or spirometry). Most were from the London COPD cohort. Two studies have multiple data points due to different measurement methods (symptom report and peak expiratory flow, Donaldson [2015] and Seemungal [2000]) over several time horizons (Seemungal [2000] at 35 days and 91 days).Abbreviations: AECOPD, acute exacerbation of chronic obstructive pulmonary disease; ED, emergency department.](/cms/asset/ecffc99b-7379-4c60-9e12-8b210b3dac8b/dcop_a_12164005_f0002_b.jpg)
