Figures & data
Table 1 Patients’ Characteristics
Table 2 Operative Procedure
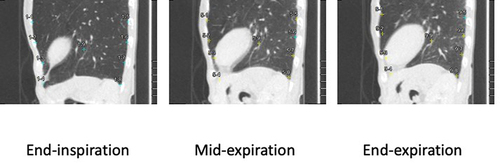
Figure 1 Example images of point placement at end-inspiration for quantitative measurement of the movement of pleura and lung field center during a single respiration, and a scheme for measured values for pleural movement and gravity-oriented distance. Example images for measurement point replacements at end-inspiration in both non-dependent and dependent pleural aspects at the costal central levels in the dependent pleural aspect and for the lung field center in the median planes, except for pulmonary apical regions, are shown on the left. Their coordinates in the remaining respiratory phases were determined by automatic tracking functions with minimal manual intervention. As shown in the scheme on the right, MPMVs in the cranial direction were defined as positive. In addition, GCR was defined as the subtracted value of the GD at peak expiration from the GD at peak inspiration divided by the GD at peak inspiration. MPMV and GCR were measured in the non-dependent and dependent pleural aspects, respectively.
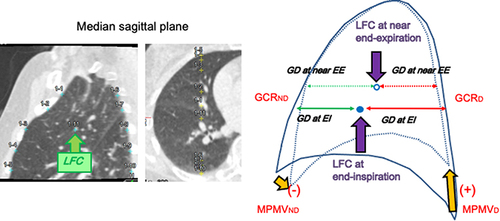
Figure 2 Comparison of MPMVND/D, GCRND/D, and MLDCR among COPD patients, non-COPD smokers, and non-smokers. Dot-plot graphs show differences in the distribution for MPMVND/D, GCRND/D, and MLDCR among patients with COPD and the non-COPD smoker and non-smoker groups. MPMVND/D was highest in the non-smoker group (0.819±0.464), followed by the non-COPD smoker group (0.405±0.131) and patients with COPD (−0.219±0.900). GCRND/D in the non-smoker group (1.003±1.384) was higher than that in patients with COPD (−0.164±1.199). MLDCR in the non-COPD smoker group (0.105±0.028) tended to be higher than in patients with COPD (0.078±0.027).
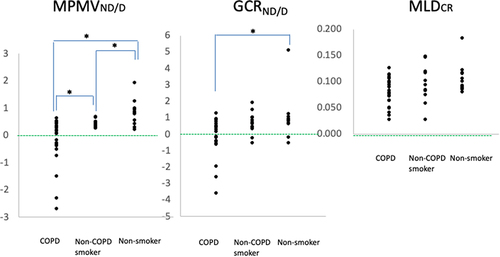
Table 3 Correlation of Measured Values with Respiratory Functional Indices and Brinkman Index
Figure 3 Correlation of MPMVND/D and GCRND/D with respiratory functional indices and Brinkman index. Scatterplot graphs for the total study population show the positive association between MPMVND/D and FEV1/FVC, with r=0.501, p<0.001 (a), the negative association between MPMVND/D and Brinkman index, with r=−0.398, p=0.006 (b), the positive association between GCRND/D and FEV1/FVC, with r= 0.445, p=0.002 (c), and the positive association between GCRND/D and FEV1 predicted, with r=0.397, p=0.006 (d). The mean values were distributed around straight lines in each graph, given by y=4.85x+69.2, y=−347x+682, y =4.03x +68.8, and y=5.34x+90.5, respectively.
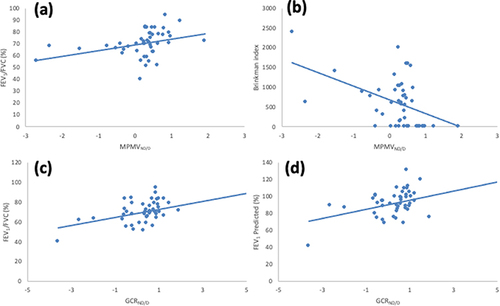
Table 4 Correlation of Mean Lung Density Parameters with Respiratory Functional Indices and Brinkman Index
Figure 4 Schematic pleural movements and gravity-oriented parenchymal collapsibility on the median sagittal plane. Schematic overview of differences in pleural movement and gravity-oriented parenchymal collapsibility among the three groups based on our results. MPMVND/D was smallest in patients with COPD, followed by the non-COPD smoker and non-smoker groups. In addition, values of MPMVND/D were negative in some patients with COPD. These results indicate that smoking is associated with a relative decrease in the movement of the non-dependent pleural aspect, and air-flow limitation can result in its paradoxical movement. In accordance with this phenomenon, parenchymal collapse during expiration in the gravitational direction for the non-dependent lung field can be impaired in patients with COPD.
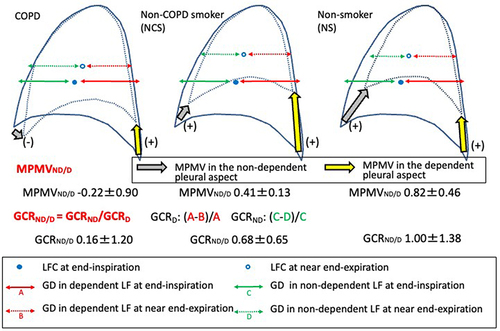
Figure 5 Example images on the median sagittal plane for the left upper lung field for three intermittent time frames in a COPD patient. Median sagittal images for the upper lung field at three intermittent time frames in an 83-year-old male patient with COPD demonstrate smaller movements in the non-dependent pleural aspect compared with the dependent pleural aspect. Moreover, the direction of the movement vector in the non-dependent pleural aspect was caudal. The MPMVND/D in this case had a negative value of −2.71. Colors of some measurement points on the pleural aspects or the lung field center at end-inspiration changed from blue to yellow at mid-inspiration and end-expiration, which means that these yellow points were located outside the displayed median sagittal plane owing to regional lateral movement.
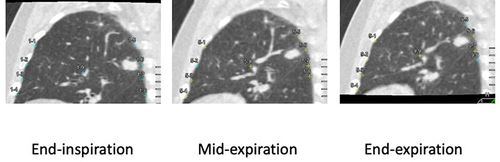
Figure 6 Example images on the median sagittal plane for the left lower lung field for three intermittent time frames in a non-COPD smoker. Median sagittal images for the lower lung field at three intermittent time frames in a 73-year-old male non-COPD smoker demonstrate much smaller movement in the non-dependent pleural aspect compared with the dependent pleural aspect. The MPMVND/D in this case had a negative value of −0.336. Colors of some measurement points on the pleural aspect or lung field center at end-inspiration changed from blue to yellow at mid-inspiration and end-expiration, which means that these yellow points were located outside the displayed median sagittal plane owing to regional lateral movement.
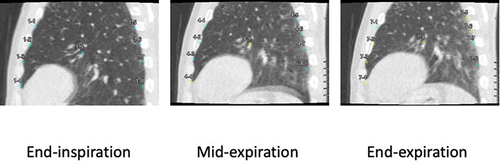
Figure 7 Example images on the median sagittal plane for the left lower lung field for three intermittent time frames in a non-smoker. Median sagittal images for the lower lung field at three intermittent time frames in an 82-year-old female non-smoker demonstrate almost comparable movements in the non-dependent pleural aspect compared with the dependent pleural aspect. The MPMVND/D in this case had a negative value of −1.24. Colors of some measurement points on the pleural aspect or lung field center at end-inspiration changed from blue to yellow at mid-inspiration and end-expiration, which means that these yellow points were located outside the displayed median sagittal plane owing to regional lateral movement.