Figures & data
Figure 1 Study design for Exacerbations and Real-World Outcomes (EROS) Among Chronic Obstructive Pulmonary Disease patients receiving BGF.
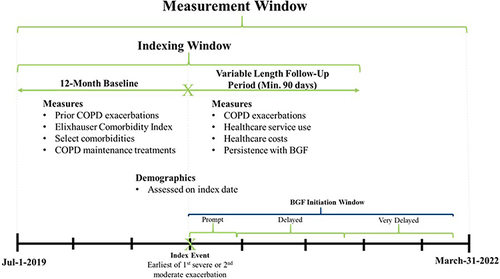
Table 1 Demographic and Clinical Characteristics, Among COPD Patients Initiating Budesonide/Glycopyrrolate/Formoterol Fumarate (BGF) Following a COPD Exacerbation, by Delay in BGF Initiation
Figure 2 Sample selection of COPD patients, initiating BGF following a COPD exacerbation.
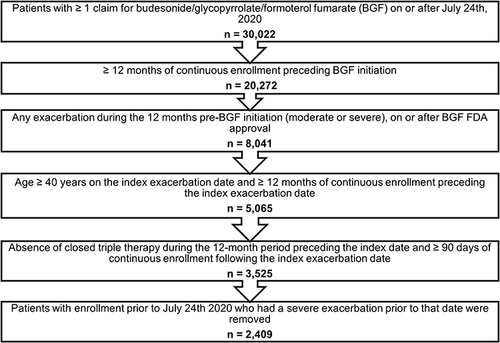
Table 2 Annualized Rates of COPD Exacerbations, Following Initiation of BGF, Among Patients Initiating BGF Following a COPD Exacerbation, by Category of Maintenance Therapy Used in the 30-Day Post-Index Period
Figure 3 Comparison of annualized rates of subsequent COPD exacerbations, following index COPD exacerbation, by delay of BGF initiation.
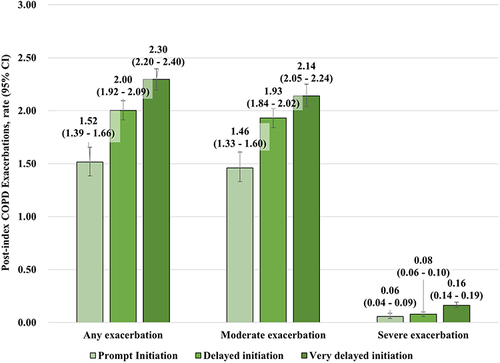
Figure 4 Adjusted rate ratios (95% confidence intervals) for average number of subsequent COPD exacerbations (per-patient-per-year) following the index exacerbation. Results for negative binomial regression model, modeling for number of post-index exacerbations, controlling for Elixhauser Comorbidity Index Score, number of baseline exacerbations, presence of short-acting treatment during baseline, presence of long-acting treatment during baseline, number of baseline COPD physician visits, number of baseline pulmonologist visits, sex, payer group (commercial, Medicare Advantage, or unknown), index exacerbation type (moderate exacerbation, moderate telehealth exacerbation, or severe exacerbation), index year (2020 or 2021), presence of baseline nebulizer use, presence of baseline oxygen therapy use, presence of baseline comorbidities, including abnormal sputum, acute bronchitis, acute respiratory failure, allergic rhinitis, anxiety, asthma, cancer diagnoses other than basal or squamous cell skin cancer, cardiovascular disease, chronic cough, COVID-19, severe COVID-19, cystic fibrosis, osteoarthritis, depression, diabetes, dyspnea, fatigue, gastroesophageal reflux disease, interstitial fibrosis, osteoporosis, pneumonia, pulmonary embolism, sarcoidosis, smoking status/tobacco, and tuberculosis. All statistically significant predictors are displayed in the figure, p < 0.05 was considered significant.
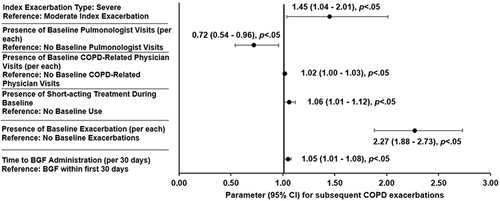
Figure 5 Estimated increase in post-index COPD exacerbations for each 3-month delay in BGF initiation, by average, (lower-bound-upper-bound) adjusted rate ratios. These estimates are extrapolated from the negative binomial regression model presented in .
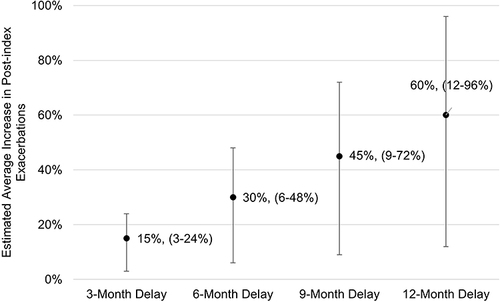
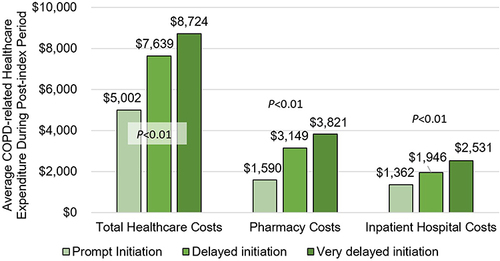
Figure 6 Average post-index COPD-related healthcare expenditure by time to BGF initiation after COPD exacerbation. Total healthcare costs include total pharmacy, physician office / clinic, emergency department, urgent care, telehealth, other outpatient, skilled nursing facility, and inpatient hospital costs. COPD-related healthcare costs are based on inpatient claims with a COPD diagnosis in the primary position, and outpatient claims with a COPD diagnosis in any position. Costs reported as per-patient-per-year (PPPY) in Q1 2022 USD.