Figures & data
Figure 1 Flow chart of patients.
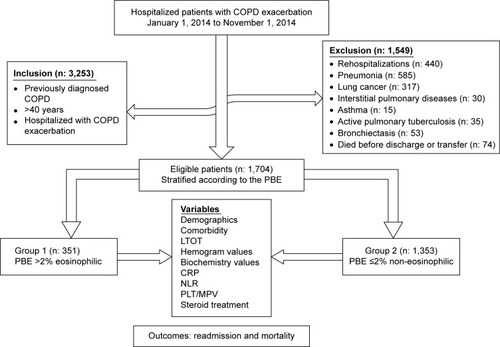
Table 1 Patients’ characteristics and laboratory findings on admission
Table 2 Laboratory findings, length of stay, and steroid use on hospital discharge
Table 3 Hospital readmission for treatment of COPD exacerbation, and mortality within 6 months after discharge
Figure 2 Eosinophilic and non-eosinophilic COPD patient survival after hospital discharge (days) as determined by Kaplan–Meier analysis.
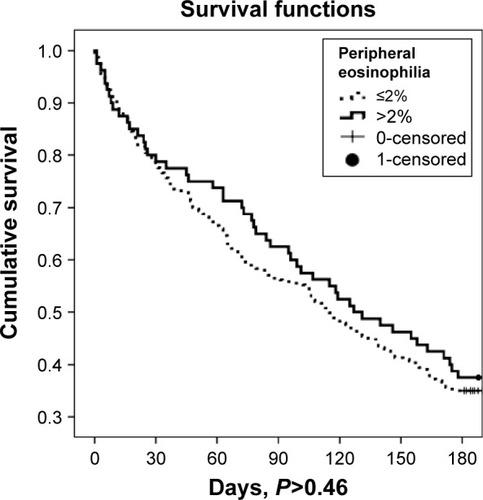
Table 4 Cox regression analysis of survival after hospital discharge
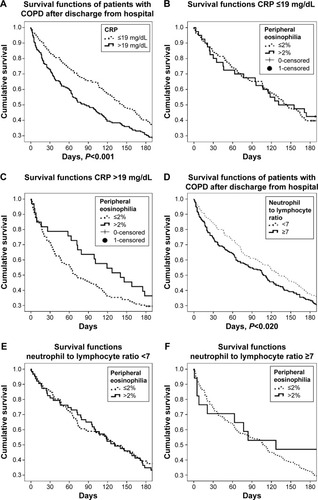
Figure 3 Survival functions of COPD patients according to CRP and NLR.