Figures & data
Table 1 Baseline Clinical, and Laboratory Characteristics of 23 Patients Prior to ICI Administration
Table 2 Baseline Clinical and Laboratory Characteristics Between Patients with Fatal and Non-Fatal ICI-Related Myocarditis, vs Other Cardiac Conditions on ICI Treatment
Figure 1 Biomarker time course in 11 patients with ICI myocarditis and lived. Time course of selected biomarkers in 11 patients with elevated troponin caused by ICI associated myocarditis. Time zero is onset of myocarditis, shown by change in myocarditis severity score from zero. Myocarditis was assigned a clinical severity score from 0–5 with 1 corresponding to symptomatic disease, 2 to symptomatic disease + abnormal biomarkers, 3 to myocarditis-related hospitalization, 4 to ICU care, and 5 assigned at the time of death. All 11 patients survived the ICI myocarditis episode displayed in this figure, although a score of 4 was reached by patient 1, 4, 8 and 9. Notable is the close association between prednisone equivalent dose score and the decline of myocarditis score as well as both laboratory and clinical indices of myocarditis. Among the important biomarkers that track with use of steroids, the QRS rose before prednisone score and declined rapidly afterwards. Lymphocyte count declined with myocarditis severity score and rose after it resolved.
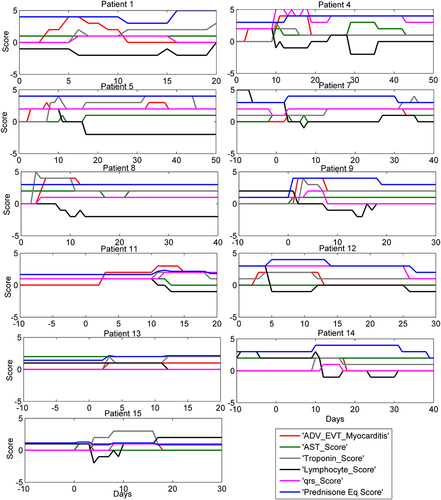
Figure 2 Biomarker time course in 4 patients with fatal ICI myocarditis. Time course of selected biomarkers in 4 patients with elevated troponin caused by ICI-related myocarditis. Time zero is onset of myocarditis, shown by change in myocarditis severity score from zero. Myocarditis was assigned a clinical severity score from 0–5 with 1 corresponding to symptomatic disease, 2 to symptomatic disease + abnormal biomarkers, 3 to myocarditis-related hospitalization, 4 to ICU care, and 5 assigned at the time of death. These 4 patients died primarily as a result of ICI myocarditis or immediate sequelae. Notable is the close association between steroid use and dose (represented in prednisone equivalents by “PrednisoneEq_Score”) and the decline of myocarditis score as well as both laboratory and clinical indices of myocarditis. However, in most cases prednisone dose was too low and started too late to be lifesaving. QRS rose before prednisone score but did not decline with inadequate prednisone dose. Lymphocyte count declined with myocarditis and did not recover with inadequate prednisone dose.
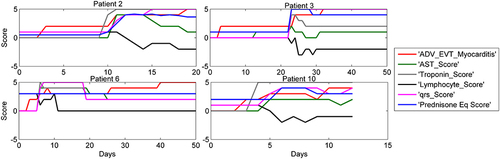
Figure 3 Biomarker time course in 8 ICI treated patients with other cardiotoxicity. Time course of selected biomarkers in 8 patients with elevated troponin that was determined not to be caused by ICI associated myocarditis. Two patients had a rise in troponin associated with worsening of CHF, 5 patients had coronary artery events primarily ischemic, and one patient had tumor hyper-progression with obstructing cardiopulmonary disease. Time zero here is the onset of troponin rise, shown by the change in troponin score. Although 3 of these cases did receive prednisone, there was seldom any evident change in the biomarkers of myocarditis, identifying these cases as not having an inflammatory cause in the heart.
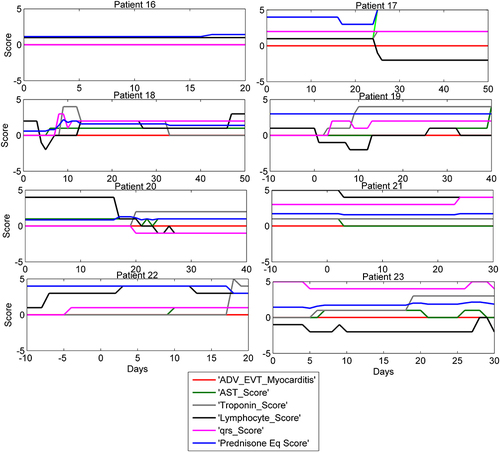
Table 3 All 23 Patients with Elevated Troponin: Comparison of Troponin and Myocarditis Score in 15 Patients with ICI-Related Myocarditis vs 8 Patients with Other Cardiotoxicity Causes for Elevated Troponin
Table 4 Model MMSE Outputs of 15 ICI-Related Myocarditis Cases, Comparing 11 Non-Fatal and 4 Fatal Cases
Figure 4 Prednisone vs myocarditis score. The averaged prednisone equivalent dose and myocarditis score are shown for patients with a response (left) and patients who did respond to treatment (right). In patients who responded, they received treatment on average 2-days earlier than patients who did not respond, and received higher doses earlier. Patients recovered from myocarditis often required prolonged high dose steroids before myocarditis scores returned to baseline.
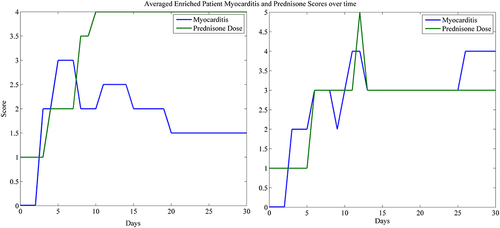
Table 5 Model MMSE Outputs for LOO Analysis of ICI-Related Myocarditis Cases, Comparing 6 Patients Who Had Clinical Resolution of Myocarditis in Response to Prednisone Treatment with 4 Non-Responder
