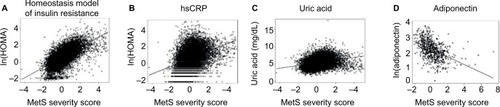
Notes: MetS severity scores and concurrent measures of (
A) homeostasis model of insulin resistance (HOMA), (
B) high-sensitivity C-reactive protein, and (
C) uric acid (all assessed among participants aged 20–64 years of the National Health and Nutrition Survey 1999–2008), and (
D) adiponectin (assessed among members of the Princeton Lipid Research cohort).
R2 values varied by race, with HOMA 0.44 for Whites and 0.36 for Blacks and Hispanics; ln(hsCRP) 0.17 for Whites and Blacks and 0.09 for Hispanics; uric acid 0.16 for Whites, 0.06 for Blacks and 0.03 for Hispanics; and adiponectin 0.22 for Whites and Blacks combined. Reprinted from
Metabolism. 63(2). Gurka MJ, Lilly CL, Norman OM, DeBoer MD. An examination of sex and racial/ethnic differences in the metabolic syndrome among adults: a confirmatory factor analysis and a resulting continuous severity score. 218–225; Copyright 2014, with permission from Elsevier,
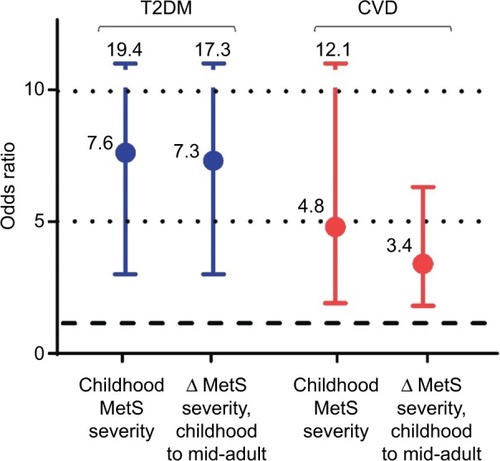
Citation61 and DeBoer MD, Gurka MJ, Morrison JA, Woo JG. Inter-relationships between the severity of metabolic syndrome, insulin and adiponectin and their relationship to future type 2 diabetes and cardiovascular disease.
Int J Obes (Lond). Epub 2016 May 24,
Citation71 with permission.
Abbreviations: hsCRP, high-sensitivity C-reactive protein; MetS, metabolic syndrome; HOMA, homeostatic model assessment.