Figures & data
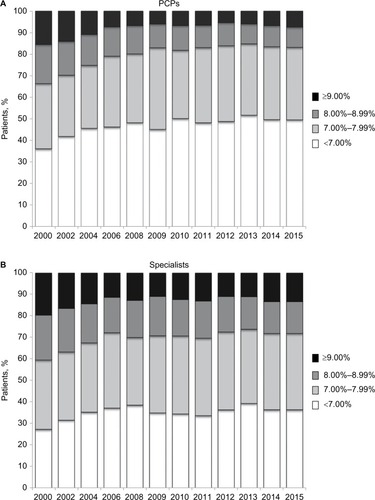
Figure 1 Analyses cohort diagram.
Abbreviations: PCP, primary care physician; T2DM, type 2 diabetes mellitus.
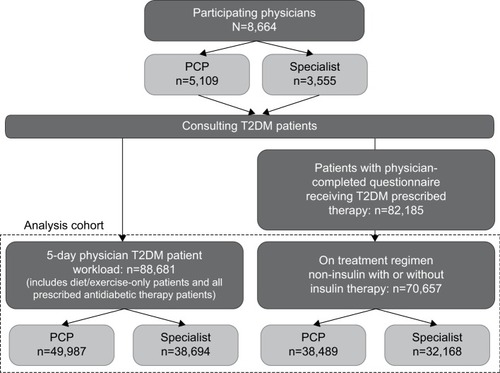
Table 1 Demographics and clinical characteristics by survey year of patients with T2DM treated by PCPs and specialists
Figure 2 Combination regimens used for the treatment of patients with T2DM between 2000 and 2015 for (A) PCPs and (B) specialists.
Abbreviations: T2DM, type 2 diabetes mellitus; PCP, primary care physician; OADs, oral antidiabetic drugs; TZDs, thiazolidinediones; SU, sulfonylurea; DPP-4, dipeptidyl peptidase 4 inhibitor; GLP-1, glucagon-like peptide 1; SGLT-2, sodium–glucose cotransporter 2 inhibitor.
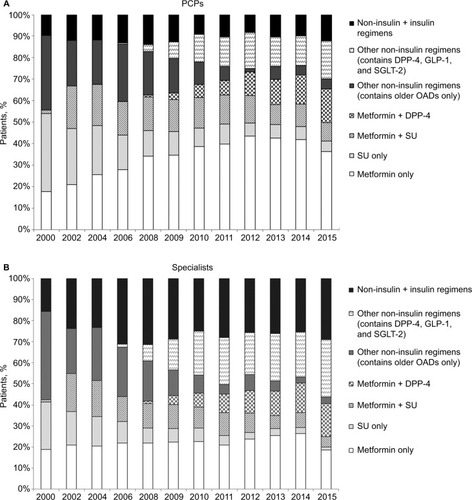
Figure 3 Time to initiation of insulin in patients with T2DM for (A) PCPs and (B) specialists.
Abbreviations: T2DM, type 2 diabetes mellitus; PCPs, primary care physicians.
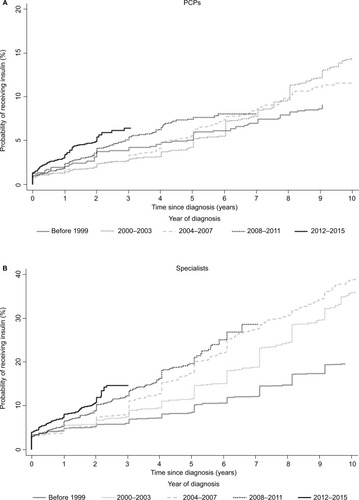
Figure 4 HbA1c levels in patients with T2DM treated by (A) PCPs and (B) specialists.
Abbreviations: HbA1c, glycated hemoglobin; T2DM, type 2 diabetes mellitus; PCPs, primary care physicians.