Figures & data
Figure 1 A simplified illustration of previously suggested angiosomes of the foot and lower ankle.
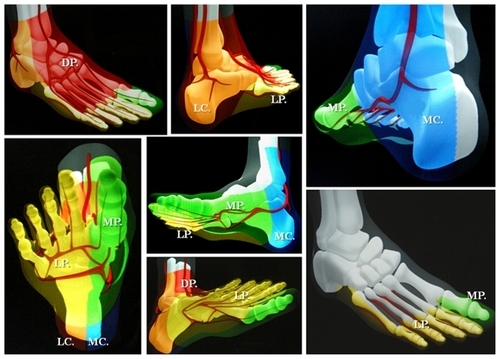
Figure 2 Selective revascularization of the posterior tibial and lateral plantar artery angiosome: (a–f) Staged angioplasties in the posterior tibial artery. (g–i) Selective angioplasties in the lateral plantar artery and its appended angiosome.
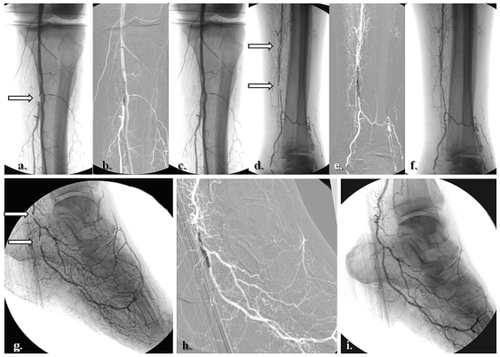
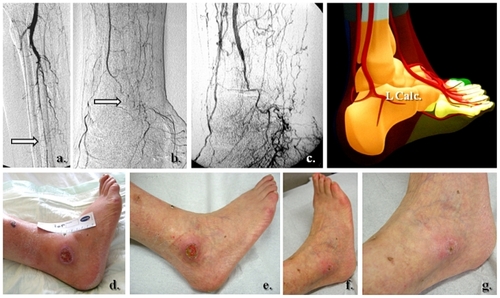
Figure 3 Clinical correspondence of the angiographic pattern showed in . A neuroischemic plantar ulcer in an acute diabetic foot presentation: (a) Initial clinical aspect featuring a lateral plantar artery hypoperfusion and sole forefoot abscess. (b) and (c) Abscess drainage and debridement. (d) and (e) Clinical evolution at weeks 3 and 5.

Figure 4 Selective revascularization of the distal posterior tibial artery and its appended medial plantar artery angiosome. (a) and (b) Selective angioplasty in the posterior tibial artery, and (c) and (d) specific revascularization of the medial plantar artery and its angiosome.
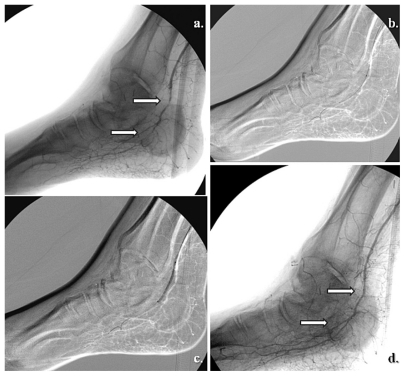
Figure 5 A right hallux neuroischemic sole ulceration matching the angiographic features showed in . There is medial plantar artery hypoperfusion in an end-artery occlusive disease pattern for the first toe. (a) Initial presentation and (b) clinical evolution at 1 month after angioplasty. (c) Results 2 months later.

Figure 6 Global medial and lateral plantar artery critical ischemia and acute diabetic foot syndrome matching staged occlusions in the posterior tibial artery (with end-artery occlusive disease model to the sole). (a) Prime posterior tibial artery staged subocclusive lesions. (b) and (c) The reestablished flow in the posterior tibial and both right plantar arteries. (d) The initial clinical aspect. (e) Subsequent evolution at 3 weeks. (f) Clinical results after 5 months of team surveillance.

Figure 7 Selective anterior tibial and related dorsalis pedis artery angiosome: (a–c) Primary staged anterior tibial angioplasty, (d) initial dorsal foot ulceration, (e) clinical results at 1 month following (f–h) associated dorsalis pedis selective angioplasty.
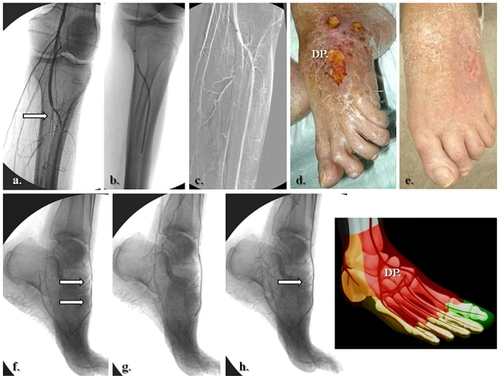
Figure 8 Specific posterior tibial and adjacent medial calcaneal artery angiosome revascularization in heel related wound. (a) Tight stenosis in the distal posterior tibial artery, above emergence of the medial calcaneal branch, (b) Angiographic result after selective angioplasty, (c) initial presentation of heel ulcer, and (d) clinical results after 5 weeks of team surveillance.
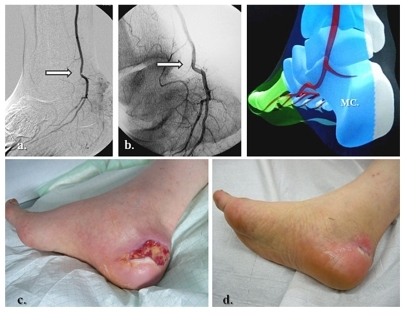
Figure 9 Lateral calcaneal artery and peroneal main flow-related angiosome ulceration. (a, b) Initial pattern of perfusion featuring the peroneal artery as single and severely diseased (end-artery occlusive model) calf vessel, (c) re-established flow in the peroneal territory, (d) prime aspect of lateral calcaneal and inframalleolar tissue defect, and (e–g) subsequent clinical evolution at weeks 1, 5, and 6.