Figures & data
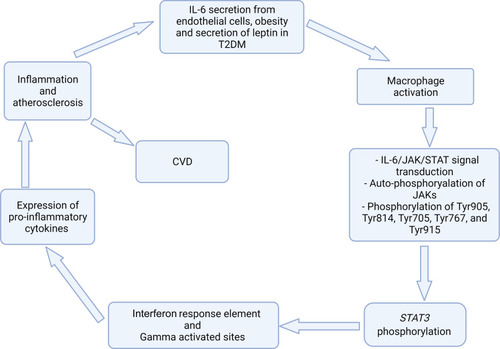
Figure 1 Leptin for progression of atherosclerosis in T2DM. The synthesis of leptin is associated with atherogenic effect because leptin receptors are found on endothelial cells. Thus, its elevation in obese individuals causes endothelial dysfunction. In this regard, obesity and secretion of leptin is a characteristic feature of T2DM. IL-6 secreted from endothelial cells activate Janus kinase/activators of transcription (JAKs) after it binds to the cytoplasmic domain of gp130 within macrophage, followed by the phosphorylation of transmembrane tyrosine receptor motifs, such as Tyr905, Tyr814, Tyr767, Tyr705 and Tyr915. This leads to increase expression of pro-inflammatory genes through STAT3, which aggravates inflammation and atherosclerosis in T2DM.
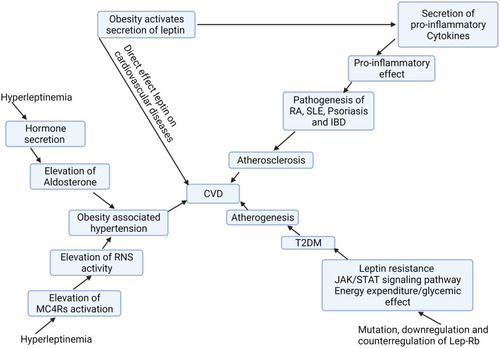
Figure 2 Cumulative effect of leptin on both chronic inflammatory disorders and further cardiovascular complication. The homeostatic role of adipose tissue impaired due to obesity-associated inflammation. The impairment of adipose tissue results in the release of effector adipokines, including leptin. The adipokines secreted by adipose tissue involve in obesity related inflammatory disorders, such as psoriasis, SLE and RA by activating of secretion of various cytokines. Conversely, obesity induced inflammation causes an impairment in sympathetic activity that controls the renin–angiotensin system through secretion of aldosterone, which results in elevation in water and salt retention and leads to obesity-associated hypertension. The reduced physiological activity of leptin on adipose tissue to oxidize stored fat leads to a phenomenon known as leptin resistance. In this regard, leptin resistance occurs in diabetic and obese subjects. Adiposity and obesity are risk factors for the occurrence of metabolic syndrome, such as T2DM and hypertension. In addition to this, RA, psoriasis and SLE are developed due to adiposity and obesity, which in turn leads to cardiovascular complications.
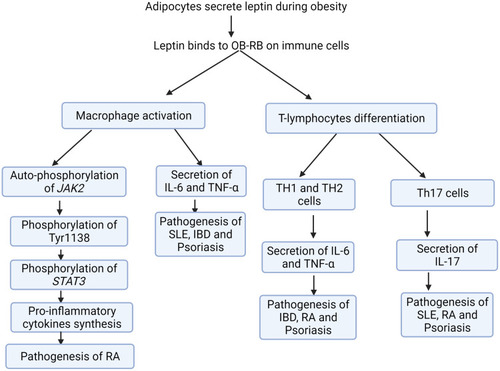
Figure 3 The impact of leptin on the pathogenesis of chronic autoimmune inflammatory disorders. Leptin binds to its long isoform receptor (Ob-RB) on macrophage to induce its biological and physiological effect through a JAK/STAT signaling pathway. This signaling cascade within macrophage induces the synthesis of pro-inflammatory cytokines, including IL-6 and TNF-α. The synthesis and release of IL-6 and TNF-α also involves the pathogenesis of RA. Similarly, IBD is one of inflammatory disorders which is characterized by elevation in the level of pro-inflammatory cytokines, including TNF-α, IL-6 and IL-1 that leads to the development of diseases. In contrast, the immune dysregulation related to leptin is due to elevated differentiation of Th17 cell, which in turn leads to tissue damage in autoimmune inflammatory disorders, including, SLE, psoriasis, and RA. The effector cell, Th17 induces inflammation by the activating secretion of IL-17 which also enhance tissue damage and inflammation in SLE. In the pathogenesis of psoriasis, studies done in mice showed that leptin induces and activates the differentiation of T-lymphocytes to T-helper-1 lymphocytes (Th1 lymphocytes) to release pro-inflammatory mediators, including TNF-α, IL-6 and IL-8.