Figures & data
Figure 1 Pancreas, intestinal tissues, and microflora in normal and T1DM conditions.
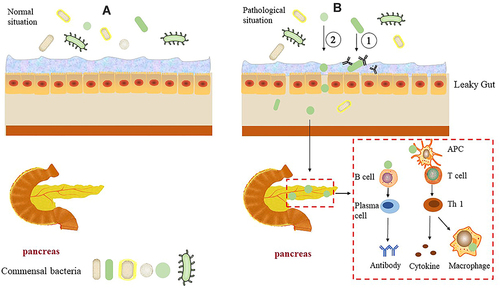
Figure 2 Communication between intestinal microbiota and immune cells.
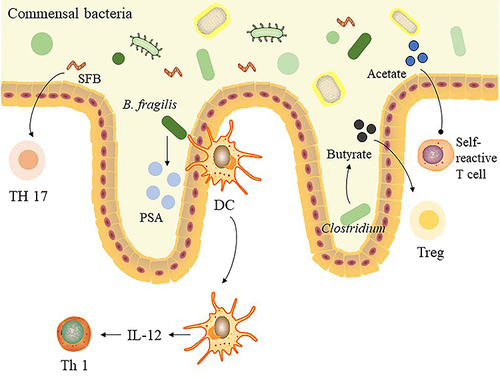
Table 1 The Effect of Treatments on Intestinal Microbiota in T1DM Clinical Trial
