Figures & data
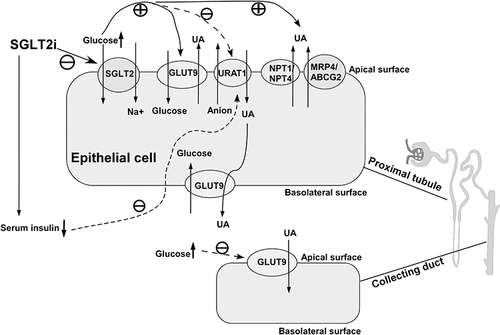
Figure 1 Exogenous and endogenous purine is deaminated to form inosine monophosphate (IMP), which can convert to adenosine monophosphate (AMP) or guanosine monophosphate (GMP) and terminally turn into xanthine through two metabolic pathways. Part of AMP is dephosphorylated to adenosine by nucleotidase, and subsequently adenosine is deaminated to inosine. Similarly, GMP is converted to guanosine by nucleotidase. Inosine and guanosine are further converted to hypoxanthine and guanine by purine nucleoside phosphorylase (PNP) respectively, followed by hypoxanthine being oxidized while guanine deaminated, both to form xanthine. Eventually, uric acid is produced through xanthine oxidized reaction by xanthine oxidase (XO).
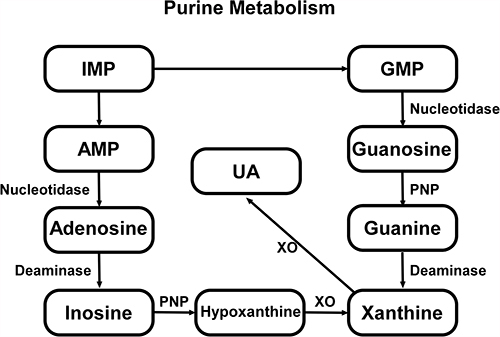
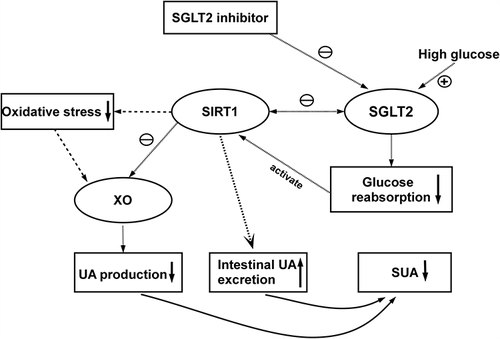
Figure 2 Transporters and proteins regulating uric acid transport in renal proximal tubule and collecting duct. OAT1 and OAT3, located on basolateral surface, are referred to as major multi-specific influx transporters that transfer uric acid from the blood to proximal tubule cells. Urate reabsorption pathway involves OAT4 and URAT1. Intracellular UA, moved by OAT4 and URAT1 from lumen, is transported through GLUT9 on basolateral membrane. ABCG-2, MRP4 and NPT1/4 on apical membrane mediate the excretion of uric acid.
Figure 3 SGLT-2i blocks SGLT-2 on apical surface resulting in increase of urinary glucose, and glycosuria subsequently stimulates excretion of uric acid transported by apical GLUT9, NPT1/NPT4 and MRP4/ABCG2. In contrast, elevated urine glucose suppresses UA reabsorption by URAT1 on apical membrane at proximal tubule and apical GLUT9 at collecting duct. In addition, SGLT-2i inhibit uric acid reabsorption by URAT1 through reducing serum insulin concentration.