Figures & data
Table 1 The Location and Function of UA Transporters in Kidney
Figure 1 Mechanism of hypothyroidism and hyperthyroidism affecting uric acid metabolism. TH can influence RBF and GFR by affecting kidney structure and function and cardiac output. With hypothyroidism, RBF and GFR decrease, resulting in reduced UA excretion and hyperuricemia occurs. On the contrary, hyperthyroidism increases RBF and GFR, resulting in increased UA excretion. However, excessive TH can promote XO activity and increase UA production, which exceeds the excretion of UA, causing hyperuricemia.
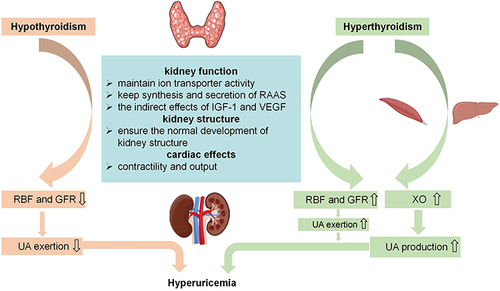
Figure 2 Obesity and IR as an essential factor in endocrine diseases with hyperuricemia. Various endocrine disorders, such as thyroid dysfunction, acromegaly, polycystic ovary syndrome and Cushing’s syndrome are frequently associated with obesity and insulin resistance (IR). IR can lead to hyperuricemia by directly affecting urate transport, stimulating ion exchange in the renal tubule and increasing lipolysis and β-oxidation. Conversely, hyperuricemia may exacerbate IR through inflammation, endothelial dysfunction and oxidative stress.
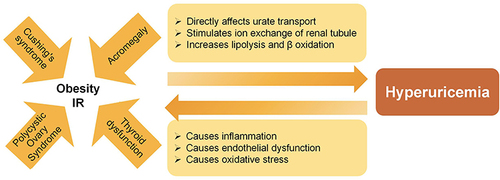
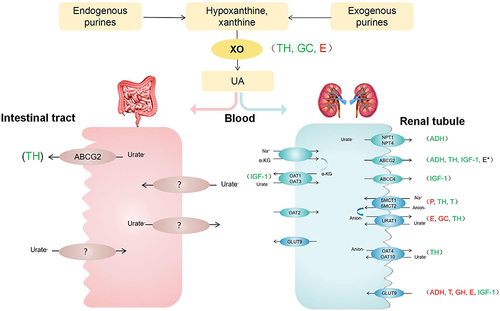
Figure 3 The effect of pituitary-target gland hormones on XO and UA transporters. Various endocrine hormones affect UA production and excretion. TH regulates the function of UA transporters such as ABCG2, SMCT, URAT1, OAT. It also could induce XO activity. E inhibits URAT1, GLUT9 and XO. About ABCG2, its function is uncertain. P inhibits SMCT1, while T promotes it. Besides, T inhibits GLUT9. GC could enhance XO activity and down-regulate URAT1. ADH is likely to promote ABCG2 and NPT1, while inhibit GLUT9. GH down-regulates GLUT9 expression. In addition, IGF-1 stimulates GLUT9, OAT1, OAT3, ABCG2 and ABCC. Green font represents promotion; Red font represents inhibition; *Represents uncertainty.