Figures & data
Figure 2 Mechanisms by which diabetic hyperglycemia can impose glucotoxicity on β cells.
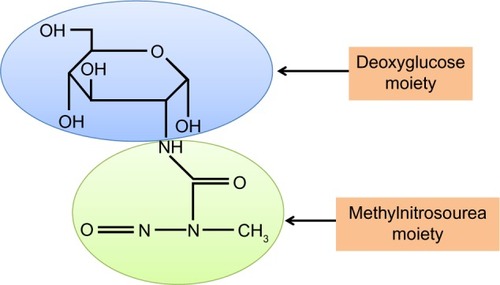
Abbreviations: STZ, streptozotocin; ROS, reactive oxygen species.
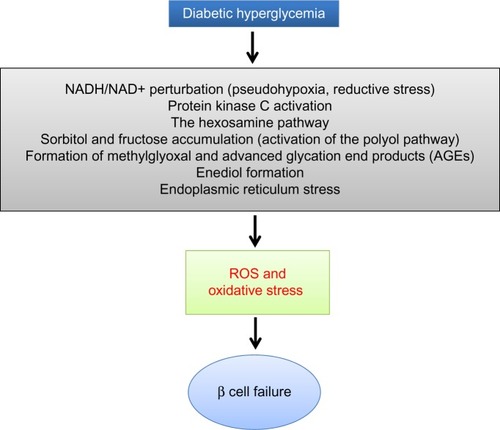
Figure 3 Glucose combustion is tightly coupled to insulin secretion in pancreatic β cells.
Abbreviation: TCA, tricarboxylic acid.
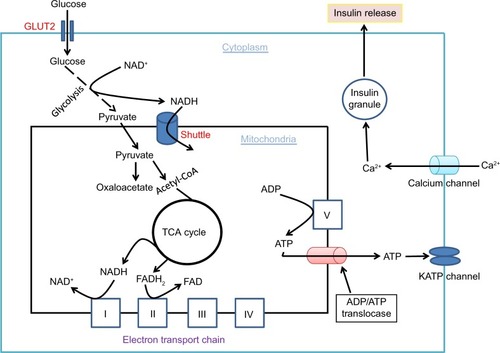
Figure 4 Role of redox imbalance between NADH and NAD+ in β cell dysfunction.
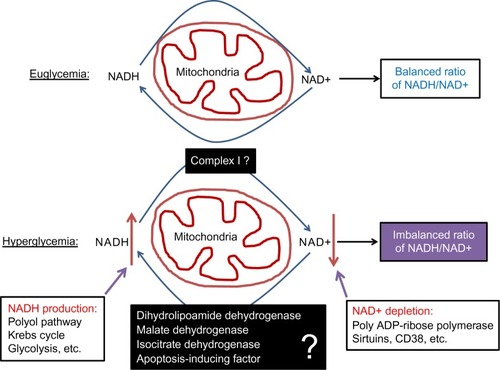
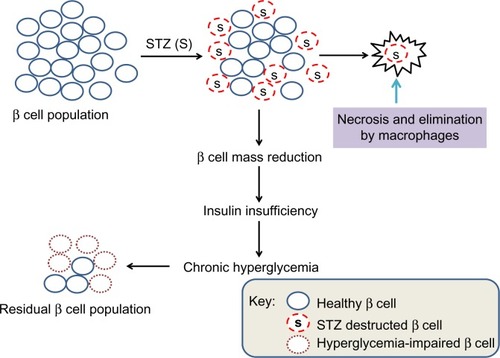
Figure 5 Scheme showing partial destruction of β cell population by STZ and reduction in β cell mass that induces insulin insufficiency and chronic hyperglycemia.
Abbreviation: STZ, streptozotocin.