Figures & data
Figure 1 Coronal-oblique MIP CT images and VR CT images of portosystemic shunts.
Abbreviations: CT, computed tomography; IILV, internal iliac vein; LRV, left renal vein; MIP, maximum intensity projection; SMV, superior mesenteric vein; VR, volume rendered.
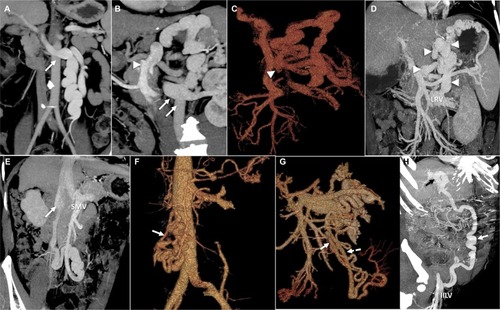
Figure 2 Circuit theory and hemodynamics of portosystemic shunts.
Abbreviations: IVC, inferior vena cava; LGV, left gastric (or coronary) vein; LRV, left renal vein; PGV, posterior gastric vein; PV, portal vein; SGV, short gastric veins; SMV, superior mesenteric vein; SV, splenic vein.
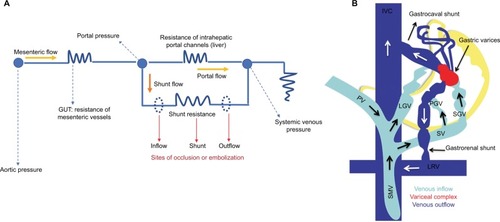
Figure 3 Interventional management of portosystemic shunt syndrome.
Abbreviations: BRTO, balloon assisted retrograde transvenous occlusion; CAATO, coil-assisted antegrade occlusion; PUV, paraumbilical vein.
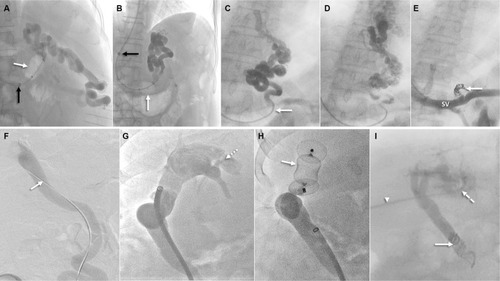
Figure 4 Balloon-assisted retrograde transvenous obliteration of lienorenal shunt.
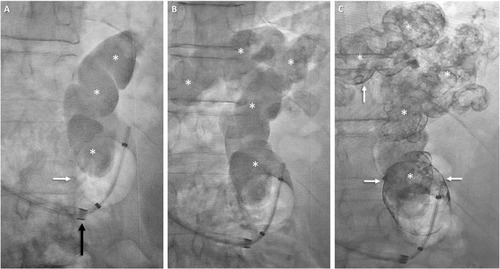
Figure 5 CARTO of mesorenal shunt in a 62-year-old male with refractory HE.
Abbreviations: CARTO, coil-assisted retrograde transvenous obliteration; HE, hepatic encephalopathy; LRV, left renal vein; MIP, maximum intensity projection.
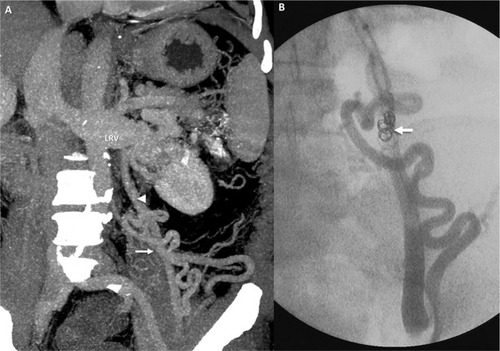
Figure 6 BRTO of a gastrolienorenal shunt in a 48-year-old male.
Abbreviations: BRTO, balloon-assisted retrograde transvenous occlusion; MIP, maximum intensity projection.
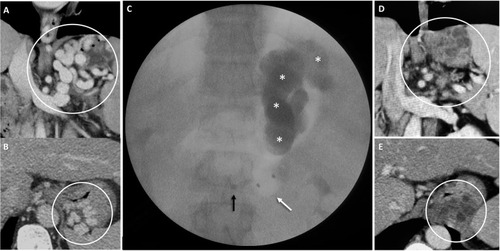
Table 1 Major studies on shunt embolization for recurrent or refractory hepatic encephalopathy
