Figures & data
Table 1 Baseline Characteristics Between Three Group Patients
Table 2 Comparison of Liver and Kidney Indexes Between Different Conditions of COVID-19 Patients
Table 3 Detailed Comparison of Liver and Kidney Indexes Between Mild Group and Severe Group
Table 4 Comparison of Clinical Laboratory Indexes Between Patients with and without Liver Injury
Table 5 Comparison of Clinical Laboratory Indicators Between Patients with and without Renal Injury
Table 6 Binary Logistic Regression Analysis of Laboratory Indexes to Predict the Mild and After-Severe Patients
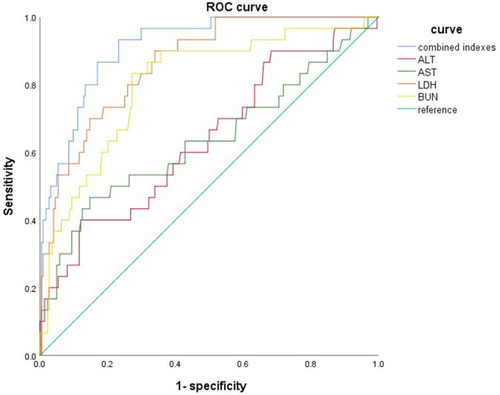
Table 7 The ROC Analysis of Liver and Kidney Indexes to Predict the Mild and Severe Patients
Figure 2 The possible mechanism of hepatocyte injury in COVID-19 patients: SARS-CoV-2 enters hepatocytes through human angiotensin converting enzyme 2(ACE2) and TMPRSS2, leading to denaturation and necrosis of hepatocytes and subsequent accumulation of bile acids. The pathogenic T cells are rapidly activated to produce proinflammatory factors such as granulocyte-macrophage colony stimulating factor (GM-CS F), interleukin (IL)-6, which induces inflammatory “storms “. And drugs may also cause drug-induced liver damage.
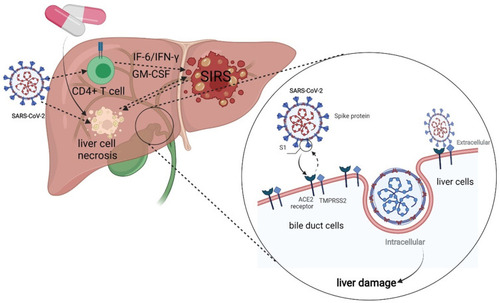
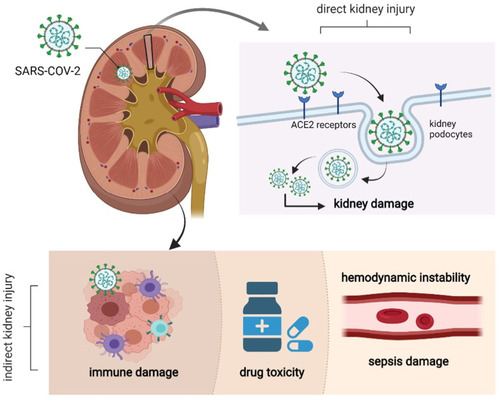
Figure 3 The possible mechanism of kidney injury in COVID-19 patients: SARS-CoV-2 enters kidney cells through human angiotensin converting enzyme 2(ACE2), resulting in degeneration and necrosis of kidney cells. Immune injury, sepsis-related kidney injury, hypovolemic renal hypoperfusion and drug-related kidney injury are all possible mechanisms of kidney injury.