Figures & data
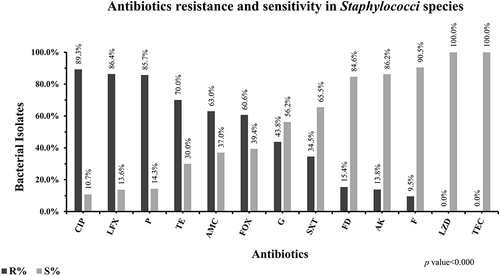
Figure 1 Distribution and prevalence of bacterial isolates in UTIs. Distribution of most prevalent (%) uropathogenic bacteria among the total number of isolates (n=572) from UTIs. Escherichia coli were the most prevalent (51.2%) among the UTIs pathogens followed by Klebsiella species (15.4%), Enterococcus species (15.4%), Pseudomonas species (9.4%), Staphylococcus aureus (3.2%), Coagulase-negative Staphylococci (CoNS) (3.0%) and Proteus species (2.4%) Bacterial isolates presented were significantly associated with UTI (p-value was < 0.000).
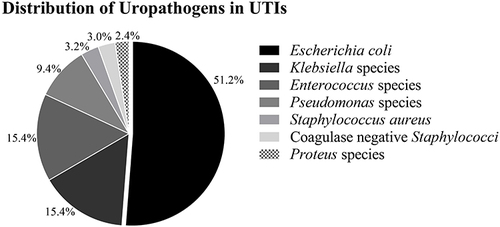
Table 1 Prevalence of Gram-Negative Rods (GNRs) and Gram-Positive Cocci (GPCs) in UTIs
Figure 2 The pattern of antibiotics resistance and susceptibility against Enterobacteriaceae. Frequency of antimicrobial resistance and susceptibility of antibiotics including ampicillin (AMP), nalidixic acid (NA), augmentin (AMC), cefotaxime (CTX), norfloxacin (NOR), ceftazidime (CAZ), co-trimoxazole (SXT), ciprofloxacin (CIP), gentamicin (G), sulbactam/cefoperazone (SCF), piperacillin/tazobactam (TZP), meropenem (MEM), imipenem (IPM), amikacin (AK), nitrofurantoin (F), fosfomycin (FOS) were presented in percentages against Enterobacteriaceae. Resistance (black bars) and susceptibility (grey bars) of all antibiotics mentioned in this graph were significantly associated with UTIs caused by bacterial isolates belonging to Enterobacteriaceae such as Escherichia coli, Klebsiella species, and Proteus species (p-value was < 0.000).
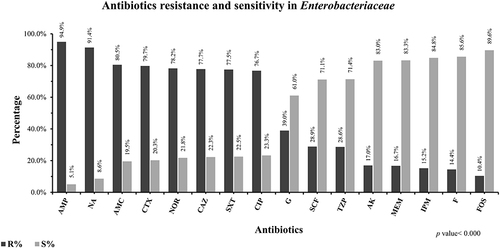
Figure 3 The pattern of antibiotics effectiveness against Pseudomonas species in UTIs. Frequency of antimicrobial resistance and susceptibility of antibiotics including norfloxacin (NOR), gentamicin (G), ciprofloxacin (CIP), ceftazidime (CAZ), cefepime (FEP), sulbactam/cefoperazone (SCF), imipenem (IPM), meropenem (MEM), amikacin (AK), piperacillin/tazobactam (TZP), colistin (CT) were presented in percentage against Pseudomonas species. Resistance (black bars) and susceptibility (grey bars) of these antibiotics mentioned in this graph were significantly associated with UTIs associated caused by Pseudomonas species (p-value was < 0.000).
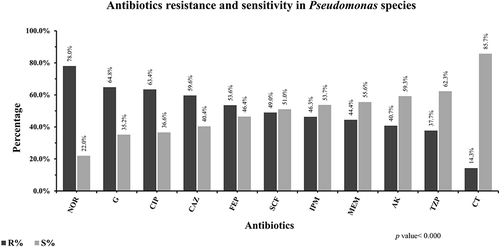
Figure 4 The pattern of antibiotics effectiveness against Enterococcus species in UTIs. Frequency of antimicrobial resistance and susceptibility of antibiotics including amikacin (AK), ciprofloxacin (CIP), gentamicin (G), augmentin (AMC), ampicillin (AMP), fosfomycin (FOS), sulbactam/cefoperazone (SCF), nitrofurantoin (F), teicoplanin (TEC), linezolid (LZD) were presented in percentage against Enterococcus species. Resistance (black bars) and susceptibility (grey bars) of all antibiotics mentioned in this graph were significantly associated with UTIs caused by Enterococcus species (p-value was < 0.000).
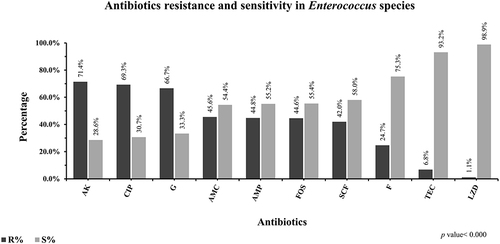
Figure 5 The pattern of antibiotics effectiveness against Staphylococci species in UTIs. Frequency of antimicrobial susceptibility of antibiotics including ciprofloxacin (CIP), levofloxacin (LFX), penicillin (P), tetracycline (TE), augmentin (AMC), fosfomycin (FOS), gentamicin (G), co-trimoxazole (SXT), fusidic acid (FD), amikacin (AK), nitrofurantoin (F), linezolid (LZD), teicoplanin (TEC) was presented in percentage against Staphylococci species. Resistance (black bars) and susceptibility (grey bars) of all antibiotics mentioned in this graph were significantly associated with UTIs caused by Staphylococci species (p-value was < 0.000).