Figures & data
Figure 1 X-ray images showed a wedge-shaped change of the L4 vertebra (A and B). T1WI of MRI demonstrated hypointense signal (red arrow) and a clear horizontal fracture line of the L4 vertebra (C), T2WI showed mixed intensity signals (red arrow) of the L4 vertebra (D), and FS-T2WI showed hyperintense signal (red arrow) and clear horizontal fracture line of L4 vertebra, quasi-circular areas of high-intensity signal around L5 vertebra was due to MRI artifact (E).

Figure 2 X-ray following vertebroplasty showed uniform distribution of bone cement in L4 vertebra (A and B). X-ray before revision surgery showed narrow intervertebral disc space at L3/4 and L4/5 with marked osteophyte formation at L3, L4, and L5 vertebra (C and D). X-ray immediately after revision surgery showed the placement of instrumentation (E and F). At 12 months after discharge, the X-ray showed no abnormal changes in instrumentation position (G and H).
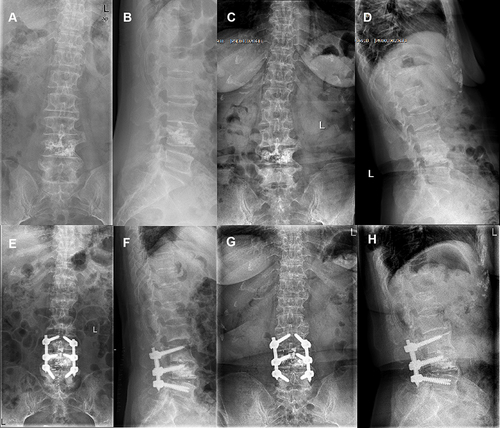
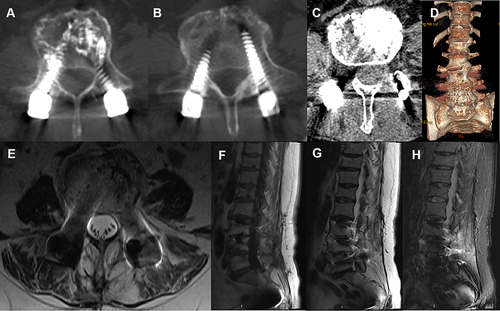
Figure 3 CT before revision surgery showed multiple bone destructive changes (red arrow) of L4 and L5 vertebra (A–D). MRI before revision surgery showed intraspinal and paravertebral abscess formation (blue arrow) of the L4 vertebra, hypointense signal (red circle) on T1WI of L3, L4, and L5 vertebra, mixed-signal intensity (red circle) on T2WI, and hyperintense signal (red circle) on FS-T2WI (E–H).
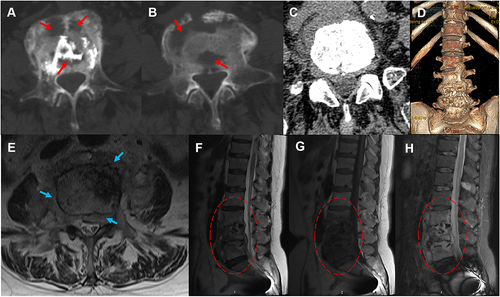
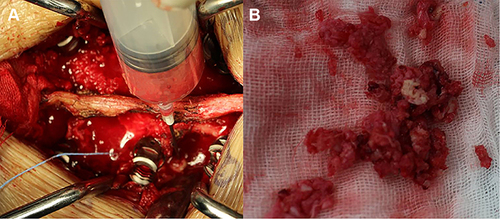
Figure 4 Intraoperative purulent fluid is seen during revision surgery (A). Disc tissue and little bone cement from L3/4 and L4/5 levels were collected during revision surgery (B).