Figures & data
Figure 1 Computed tomography scan revealing a right maxillary sinusitis (A) and left focal basal pneumonia without cavitation (B), due to Actinomyces spp., in an immunosuppressed woman.
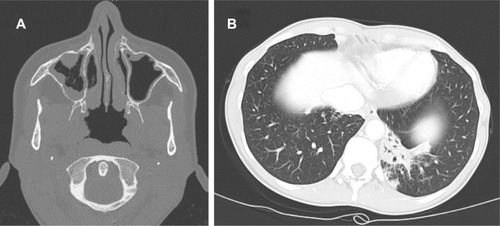
Figure 2 Chest X-ray (A) and thorax computed tomography scan (B–C) revealing multifocal pneumonia with right pleural cavitation due to Actinomyces viscosus.
Note: Arrows indicate chest wall sinus tract.
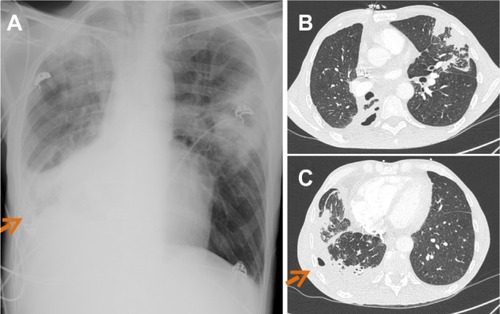
Figure 3 Panoramic dental X-ray showing right mandibular osteomyelitis (“lumpy jaw syndrome”).
Notes: An unfavorable outcome resulted, despite dental extraction of tooth 46 (with arrow showing mandibular thickening with lucencies) (A), followed by tooth 45 2 months later (B). Surgical debridement and decortication were required due to extension of the osteomyelitis to the gonial angle and to the ramus (with arrow showing the typical radiologic aspect of lumpy jaw syndrome) (C).

Figure 4 Left mandibular osteomyelitis with bone exposure (A) and sinus tract (B) following left mandibular radiotherapy in a patient receiving long-term bisphosphonate therapy. Panoramic dental X-ray shows mandibular lucencies (C).
Note: The arrow shows mandibular lucencies.
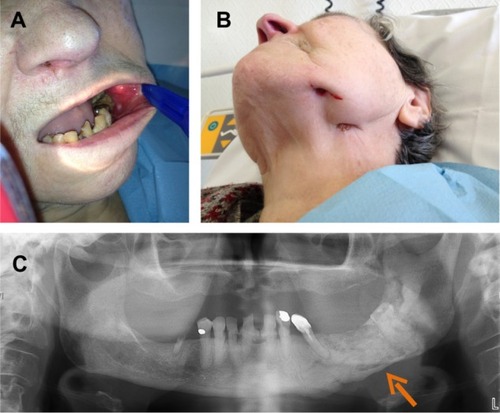
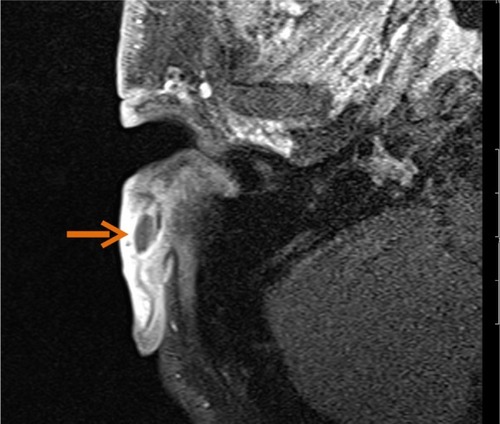
Figure 5 Contrast-enhanced magnetic resonance images showing contiguous spread of pulmonary actinomycosis to the spine (case 2), with thoracic spondylitis of the T3 vertebral body, associated with anterior paravertebral abscess (arrow) (A). Magnetic resonance image showing back soft tissue infiltration, with posterior epiduritis and infection of L2 and L4 vertebral bodies (arrows) in a paraplegic patient with plurimicrobial bone and joint infection following chronic back scar (case 6) (B).
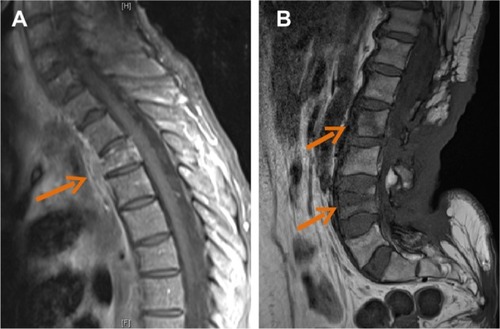
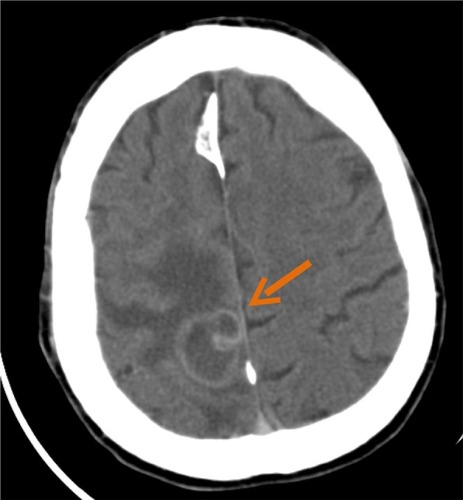
Figure 6 Abdominal computed tomography scan showing peritoneal effusion and heterogeneous pelvic mass surrounding an intrauterine device (A), with abscesses (B) corresponding with pelvic actinomycosis.

Figure 7 Abdominal computed tomography scan of a patient with evidence of actinomycosis on pathology.
Notes: Enterocutaneous fistula (arrow) (A) was associated with large intra-abdominal abscess (arrow) (B).
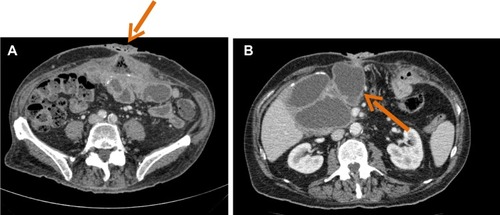
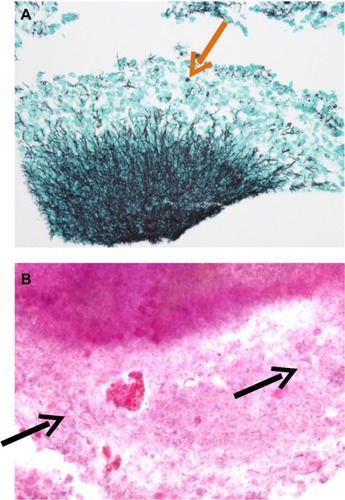
Figure 8 Pathology of a suppurative lesion in a patient with an abdominal wall implant.
Notes: Aggregates of Actinomyces spp. and sulfur granules (arrow) after silver staining (A); filamentous bacteria (arrows) after Gram staining (B).