Figures & data
Figure 2 The changes of six major NTM strains from 2019 to 2021. The number of patients infected with each strain of NTM annually from 2019 to 2021 was shown in (A–C). The ratio of males to females in each strain of NTM for each year was displayed (a–c).
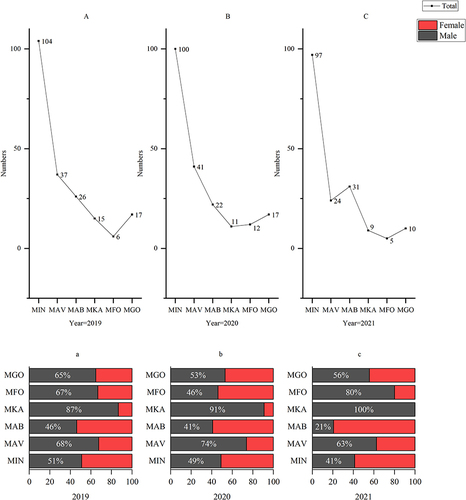
Table 1 Gender and Age of Patients Infected with NTM
Table 2 Gender Distribution Among Different Species Types
Figure 3 MICs distributions of M. abscessus and M. intracellulare to bedaquiline, clofazimine, linezolid, delamanid and pretomanid. (A) The MIC distributions of M. abscessus against bedaquiline. (B) The MIC distributions of M. intracellulare against bedaquiline. (C) The MIC distributions of M. abscessus against clofazimine. (D) The MIC distributions of M. intracellulare against clofazimine. (E) The MIC distributions of M. abscessus against linezolid. (F) The MIC distributions of M. intracellulare against linezolid. (G) The MIC distributions of M. abscessus against delamanid. (H) The MIC distributions of M. intracellulare against delamanid. (I) The MIC distributions of NTM against pretomanid. The position indicated by the arrow indicates the critical concentration value of resistance.
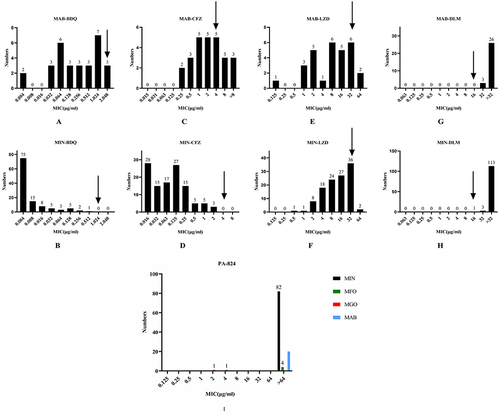
Table 3 NTM Mutation M. abscessus of BDQ, CFZ, and LZD
Table 4 NTM Mutation M. Intracellulare of LZD