Figures & data
Table 1 Patient Demographics and Microbiological Data in Four Pediatric Patients with Mucormycosis
Figure 1 (A–E) Magnetic resonance imaging of patient No. 2. (A) The left occipital lobe showed an irregular gyrus with an abnormal signal shadow and a low signal on T1WI (arrow). (B) Slightly high signal on T2WI (arrow). (C) Slightly high signal on FLAIR (arrow). (D) Limited DWI diffusion (arrow). (E) Limited DWI diffusion (arrow). (F) Computed tomography (CT) of patient No. 1 showing multiple pulmonary nodules and marginal halo sign (arrow). (G) Computed tomography (CT) of patient No. 1 showing air crescent sign (arrow). (H) Enhanced CT of patient No. 3 showing left pulmonary artery occlusion, left atelectasis and left pleural effusion (arrow). (I) Enhanced CT of patient No. 3 showing left pulmonary vein occlusion (arrow). (J) Enhanced CT of patient No. 1 showing aortic arch dissection with ruptured pseudoaneurysm (arrow). (K) Enhanced CT of patient No. 4 showing a pseudoaneurysm of the descending aorta (arrow). (L) Bronchoscope of patient No. 4 showing a grayish-brown necrotic mass occluding the middle lobe of the right lung (arrow). (M) Bronchoscope of patient No. 1 showing a gelatinous substance occluded the base lobe of the left lower lung (arrow). (N) Alveolar lavage fluid pathology of patient No. 3 showing typical hyphal morphology. Mucorales hyphae were at least 6–16 µm wide, ribbon-like, pauci-septate, with subrectangular branching (HE 20X). (O) Alveolar lavage fluid pathology of patient No. 3 showing typical hyphal morphology. Mucorales hyphae were at least 6–16 µm wide, ribbon-like, pauci-septate, with subrectangular branching (PASM 20X).
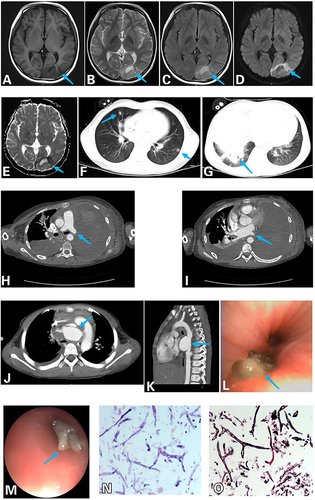
Table 2 Treatments and outcomes of Four Pediatric Patients with Mucormycosis
Data Sharing Statement
The key information and data generated and analyzed during this are given in this article.
