Figures & data
Table 1 Baseline Characteristics of Participants
Table 2 Univariate Analysis for SYNTAX Score
Table 3 Relationship Between GHbA1c and SYNTAX Score in Different Models
Table 4 Threshold Effect Analysis of GHbA1c and SYNTAX Score Using Piece-Wise Linear Regression
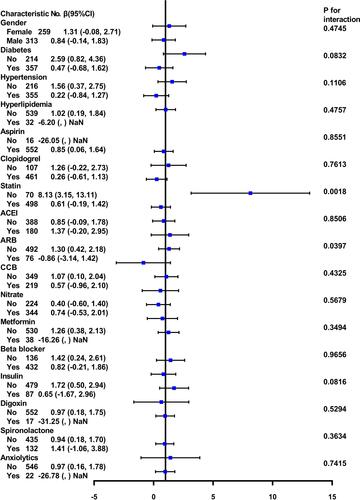
Figure 1 Association between GHbA1c and SYNTAX score in coronary heart disease patients. A threshold, nonlinear association between GHbA1c and SYNTAX score was found (P=0.0052) in a generalized additive model (GAM). Solid red line represents the smooth curve fit between variables. Blue bands represent the 95% of confidence interval from the fit. All adjusted for age, gender, BMI, TG, TC, LDL-C, HDL-C.
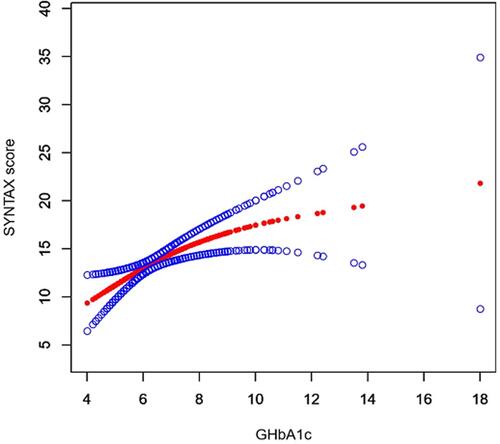
Figure 2 The interacting and stratified analyses of affecting the association between HbA1c and SYNTAX score. Adjusted for season of age, BMI, SBP, DBP, TC, TG, LDL-C, HDL-C, UA, Cr, ALT except the variable. Small number of interactions were observed based including: the medication history of statins and ARBs (P values for interaction <0.05). In this study, the stronger association of HbA1c and SYNTAX score were detected in no diabetes, hypertension, hyperlipidemia status, and no previous medication history of statins, ARBs, CCBs, metformin, beta blockers, insulin, digoxin, spironolactone, anxiolytics (<0.05P). In contrast, the weaker association was detected between men and female with disease history of diabetes, hypertension, and with previous medication history of statins, ARBs, CCBS, beta blockers, insulin, spironolactone, with and without the medication history of clopidogrel, nitrates, ACEIs.(,) NaN: the model failed because of the small sample size.