Figures & data
Table 1 Patient Characteristics
Table 2 Patient Characteristics of the Group A with No Mediastinal Widening
Table 3 Patient Characteristics of Group B with Mediastinal Widening
Figure 1 Computed tomography (CT) images of the chest of a 75-year-old woman with systemic lupus erythematosus and Sjogren syndrome. CT performed at admission revealed consolidation and reticular opacities in peripheral areas of both lungs (A). A CT scan performed 1 month later revealed the appearance of gas density in the anterior mediastinum (white arrow) and around the carina (black arrow) (B). The width of the anterior mediastinum decreased owing to weight loss.
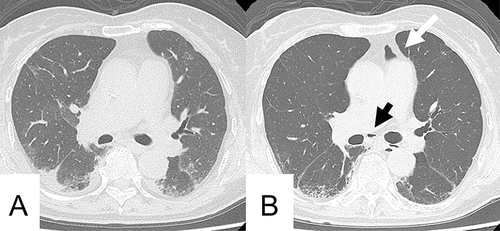
Figure 2 Computed tomography (CT) images of the chest of an 89-year-old man with idiopathic pulmonary fibrosis (IPF). CT performed 1 year ago revealed reticular opacities and honeycombing in peripheral areas of both lungs consistent with IPF (A). A CT scan performed on admission revealed that the reticular opacities and honeycombing were exacerbated (B). Pneumomediastinum appeared around the pulmonary artery (arrows); however, no enlargement of the mediastinum was observed.
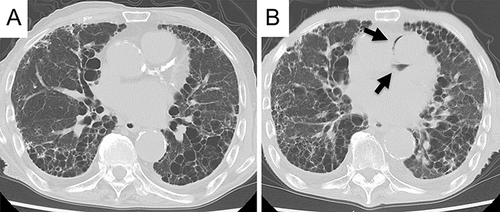
Figure 3 The balance between the pressures in the intrathoracic cavity and the mediastinum in a normal chest. When the intrapleural space pressure rises, a positive pressure pneumomediastinum develops to balance the difference. Similarly, negative pressure pneumomediastinum occurs to abolish the pressure difference when the mediastinal pressure decreases.
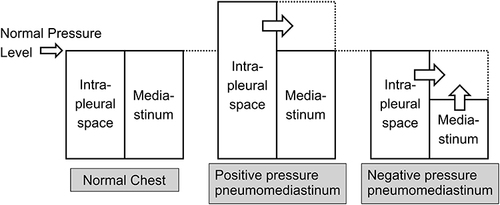
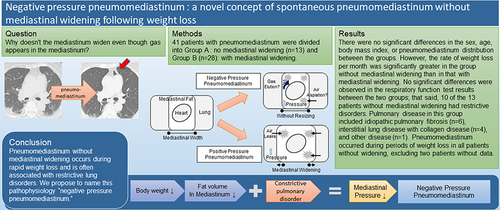
Figure 4 Pathophysiology of positive and negative pressure pneumomediastinum. Increased intrapleural pressure (A) causes air leaks, resulting in positive pressure pneumomediastinum. Mediastinal fat decreases with weight loss (B) resulting in mediastinal narrowing because the lungs replace the space. In patients with restrictive lung disorder due to interstitial lung disease, mediastinal resizing does not occur owing to reduced plasticity. This reduces the mediastinal pressure and causes pneumomediastinum without mediastinal resizing (C).
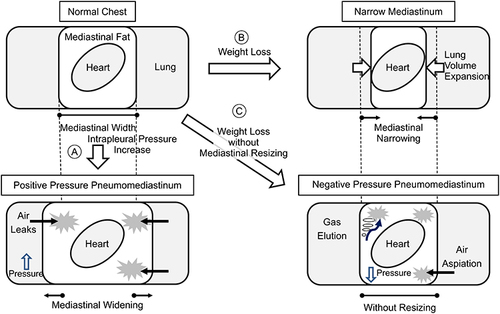
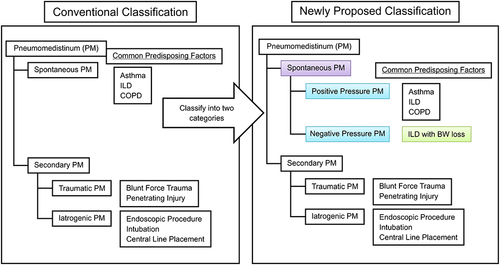
Figure 5 Newly proposed classification for spontaneous pneumomediastinum (PM). PM is classified as spontaneous PM and secondary PM. Spontaneous PM can be divided into the following two categories: positive pressure PM that represents conventional spontaneous PM and the new additional category of negative pressure PM. BW, body weight; COPD, chronic obstructive pulmonary disease; ILD, interstitial lung disease.