Figures & data
Figure 1 Complex entanglement of the umbilical cord following delivery by Emergency Cesarean Delivery for intrapartum non-reassuring fetal heart rate, during spontaneous labor at 40 and 5/7 weeks’ gestation. Note the true knot of the umbilical cord located within multiple loops of nuchal cord. Also note particulate meconium-stained amniotic fluid.

Figure 2 Sagittal imaging of the fetal neck. Fetal cranium is to the right of the image. Real-time sonography depicting a quadruple nuchal cord. Note the prominent “divot sign” representing marked subcutaneous indentation of the fetal skin overlying the posterior aspect of the fetal neck, exerted by pressure of the four loops of nuchal cord upon the fetal neck. Also note that each of the larger umbilical veins is accompanied by two (smaller caliber) umbilical arteries, respectively.

Figure 3 Sagittal imaging of the fetal neck. Power Doppler imaging depicting a quadruple nuchal cord depicted in . Note that each of the larger umbilical veins is accompanied by two (smaller caliber) umbilical arteries, respectively.

Figure 4 Sagittal image of the fetal neck. Fetal cranium is to the right of the image. Power Doppler depicting a triple nuchal cord.

Figure 5 Sagittal imaging of the fetal neck. Fetal cranium is to the right of the image. Power Doppler imaging depicts coexisting true knot of the umbilical cord located within a nuchal cord (note the umbilical vein and two arteries seen “en face” within the almost complete umbilical cord circle). Reproduced from Sherer DM, Dalloul M, Ward K, et al. Coexisting true umbilical cord knot and nuchal cord: possible cumulative increased risk of adverseperinatal outcome. Ultrasound Obstet Gynecol. 2017;50(3):404–405. Copyright © 2016 ISUOG. Published by John Wiley & Sons Ltd.Citation34

Figure 6 Power Doppler imaging of complex umbilical cord entanglement in monochorionic monoamniotic twins at 27 weeks’ gestation.

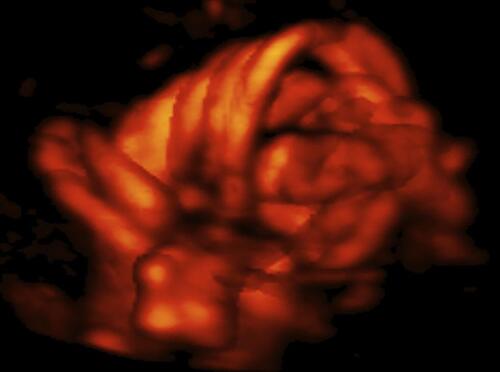
Figure 7 Three dimension (3D) color Doppler imaging of complex umbilical cord entanglement in monochorionic monoamniotic twins at 27 weeks’ gestation.
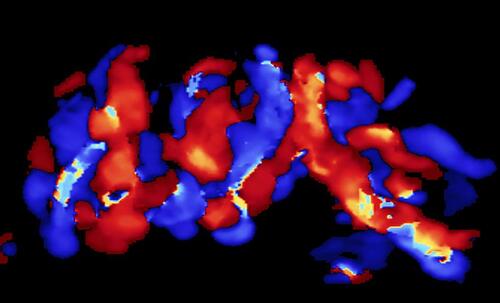
Figure 8 Three dimension power (3D) Doppler imaging of complex umbilical cord entanglement in monochorionic monoamniotic twins at 27 weeks’ gestation. The monoamniotic twins depicted in –8 were delivered by emergency Cesarean at 29 and 1/7 weeks’ gestation, due to prolonged fetal bradycardia of twin B (60 bpm for 14 minutes), one day after admission for continuous fetal heart rate monitoring and intramuscular rescue steroids to decrease overall prematurity-associated neonatal morbidities should premature delivery become indicated. At delivery, marked entanglement of the umbilical cords and complex umbilical cord entanglement of twin B (a true knot and nuchal cord), were noted. Birth weights were 1195 and 1385 grams, respectively; Apgar scores were 5/7/9 and 6/8/9 at 1, 5 and 10 minutes, respectively, and umbilical artery gas analyses; pH = 7.27 base excess = −3.4 and 7.22 and −4.6, for twins A and B, respectively. Both infants did well.