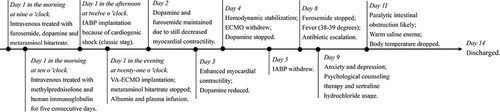
Figures & data
Figure 1 The dynamic changes of electrocardiogram and chest radiograph. (A) Electrocardiogram (ECG) showed QS complex only in V1-V3 leads and 1–2 mm ST-segment depression in II, III, aVF, V4-V6 leads on April 13th. (B) Chest radiograph showed bilateral pulmonary scattered inflammatory changes and possible pulmonary on April 13th. (C) Discordant terminal negative T waves in leads V1–V6 was observed in ECG on April 18th. (D) Chest radiograph showed no pulmonary congestion and obvious inflammation on April 19th.
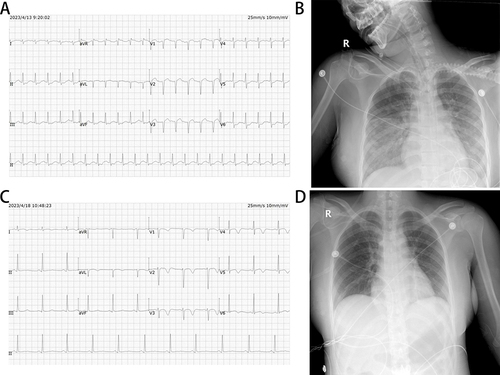
Figure 2 The transthoracic echocardiography (TTE). (A) TTE on April 13th revealed severely impaired movement of the ventricular wall (left ventricular end diastolic diameter (LVEDD), 47.3 mm; interventricular septum thickness (IVS), 8.4 mm; left ventricular ejection fraction (LVEF), 35.7%; left ventricular fraction shortening (LVFS), 17.1%; stroke volume, 37.1 mL), moderate to severe regurgitation of the mitral valve and tricuspid valve (the estimated pulmonary artery systolic blood pressure was 49 mmHg) and deteriorated diastolic function (E/E′, 9.1) as well as a moderately reduced right ventricular function [tricuspid annular plane systolic excursion (TAPSE), 12 mm]. The inferior vena cava was widened (inferior vena cava diameter, 22.3 mm]) and its’ respiratory collapse rate was less than 50%. (B) TTE on April 14th still showed decreased myocardial contractility (LVEDD, 51.9 mm; IVS, 8.0 mm; LVEF, 36.6%; LVFS, 17.7%; stroke volume, 47.3 mL), severe regurgitation of the mitral valve and deteriorated diastolic function (E/A, 3.3; E/E′, 21.5) as well as a moderately reduced right ventricular function. The respiratory collapse rate of inferior vena cava (diameter, 17.2 mm) was less than 50%. (C) TTE on April 21th revealed a normalized cardiac function (LVEDD, 42.5 mm; IVS, 10.5 mm; LVEF, 50.8%; LVFS, 30.3%; stroke volume, 46.9 mL), moderate regurgitation of the mitral valve and restored diastolic function (E/A, 1.8; E/E′, 9.7) without reduced right ventricular function.
![Figure 2 The transthoracic echocardiography (TTE). (A) TTE on April 13th revealed severely impaired movement of the ventricular wall (left ventricular end diastolic diameter (LVEDD), 47.3 mm; interventricular septum thickness (IVS), 8.4 mm; left ventricular ejection fraction (LVEF), 35.7%; left ventricular fraction shortening (LVFS), 17.1%; stroke volume, 37.1 mL), moderate to severe regurgitation of the mitral valve and tricuspid valve (the estimated pulmonary artery systolic blood pressure was 49 mmHg) and deteriorated diastolic function (E/E′, 9.1) as well as a moderately reduced right ventricular function [tricuspid annular plane systolic excursion (TAPSE), 12 mm]. The inferior vena cava was widened (inferior vena cava diameter, 22.3 mm]) and its’ respiratory collapse rate was less than 50%. (B) TTE on April 14th still showed decreased myocardial contractility (LVEDD, 51.9 mm; IVS, 8.0 mm; LVEF, 36.6%; LVFS, 17.7%; stroke volume, 47.3 mL), severe regurgitation of the mitral valve and deteriorated diastolic function (E/A, 3.3; E/E′, 21.5) as well as a moderately reduced right ventricular function. The respiratory collapse rate of inferior vena cava (diameter, 17.2 mm) was less than 50%. (C) TTE on April 21th revealed a normalized cardiac function (LVEDD, 42.5 mm; IVS, 10.5 mm; LVEF, 50.8%; LVFS, 30.3%; stroke volume, 46.9 mL), moderate regurgitation of the mitral valve and restored diastolic function (E/A, 1.8; E/E′, 9.7) without reduced right ventricular function.](/cms/asset/e239a739-4088-4211-9c29-ea9a1df0d53f/dimc_a_12300299_f0002_c.jpg)
Figure 3 The Coronary angiography. Coronary angiography revealed that there was no stenosis or obstructive lesions in the coronary artery April 13th.
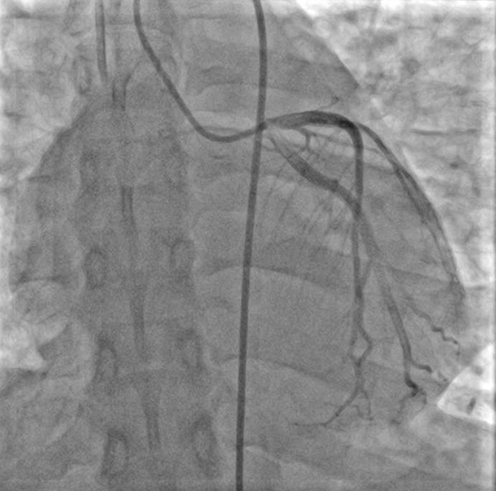
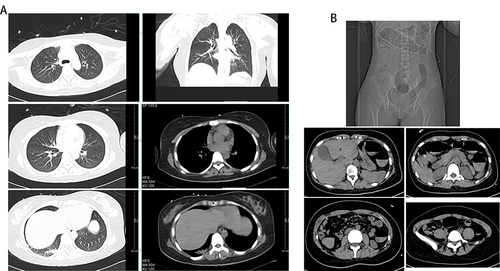
Figure 4 The lung and abdominal computerized tomography. (A) Lung computerized tomography showed scattered streaks in the right lower lung April 21th. (B) Full abdominal computerized tomography scan revealed that colorectal dilatation, which need being ware of paralytic intestinal obstruction April 24th.