Figures & data
Figure 1 CLL transformation into DLBCL.
Abbreviations: CLL, chronic lymphocytic leukemia; DLBCL, diffuse large B-cell lymphoma; HE, hematoxylin and eosin.
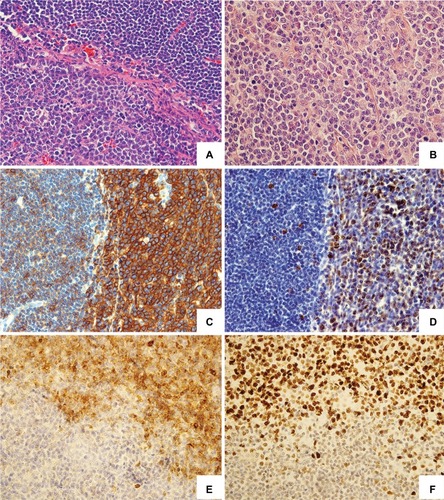
Figure 2 Morphological and phenotypic spectrum of CLL transformation into HL may strongly differ upon histopathological examination.
Abbreviations: CLL, chronic lymphocytic leukemia; HE, hematoxylin and eosin; HL, Hodgkin’s lymphoma; HRS cell, Hodgkin and Reed–Sternberg cell.
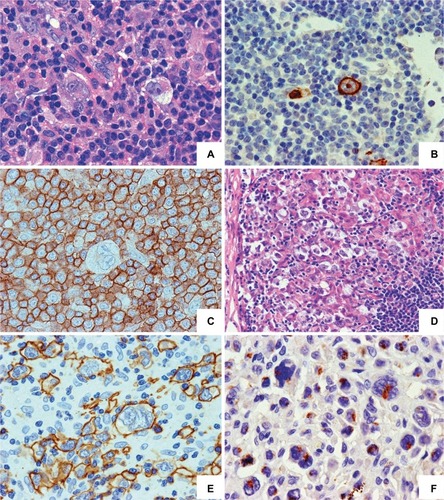
Figure 3 Management algorithm for patients with a clinical suspicion of RS.
Abbreviations: ABVD, adriamycin, bleomycin, vinblastine, and dacarbazine; CLL, chronic lymphocytic leukemia; DLBCL, diffuse large B-cell lymphoma; HSCT, hematopoietic stem cell transplantation; LDH, lactate dehydrogenase; PET/CT, positron emission tomography/computed tomography; R-CHOP, rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; RS, Richter syndrome; SUV, standardized uptake value.
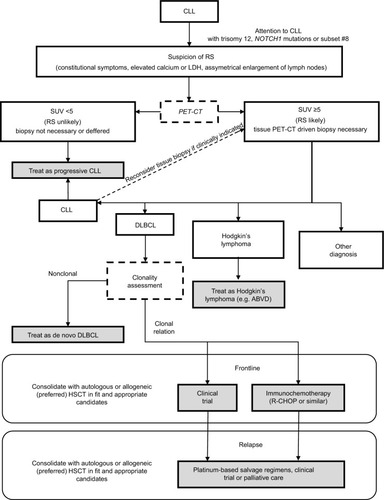
Table 1 Summary of the published retrospective studies assessing the efficacy and safety of induction regimens for patients with DLBCL-RS
Table 2 Summary of the published prospective studies assessing the efficacy and safety of induction regimens for patients with DLBCL-RS
