Figures & data
Figure 1 There are three aspects to the cellular and chemical pathology of asthma: the epithelial and subepithelial response the subsequent inflammatory process; and the impact on airway mucus and bronchoconstriction. When children with asthma inhale an aeroirritant, there is a complex interplay of cells and chemical that is poorly understood. The main chemical players are called “alarmins”, and these link with cells such as Antigen-Presenting Cells and Dendritic Cells. These drive a shift in the types of T-cells that a person has. In most people with asthma there is an imbalance such that the undifferentiated T-helper cell (Th-0) is more likely to become a Th2, rather than Th1, cell. When this happens, people are said to have “Type 2-high” asthma; this is the usual phenotype in children. There are two main asthma endotypes in children with Type 2-high asthma - the eosinophilic pathway, and the IgE-mediated pathway. The key chemicals that drive these pathways include Interleukin 4/13 and Interleukin-5. Children exhibit these pathways and endotypes to varying degrees. There are other aspects of the pathogenesis, such as Th-17, which promote non-Type 2 inflammation. The consistent driver in children with Type 2-high asthma is that avoidance of aeroirritants in the first place significantly reduces the inflammatory load.
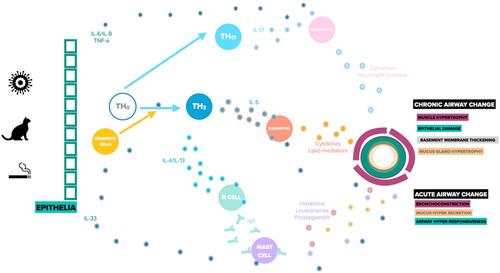
Table 1 A Summary of Risks for Development of Childhood Asthma in Relation to Exposure to Allergens Described in This Review. (Based on Dick et al)Citation28
