Figures & data
Table 1 Clinical Characteristics of the Study Population
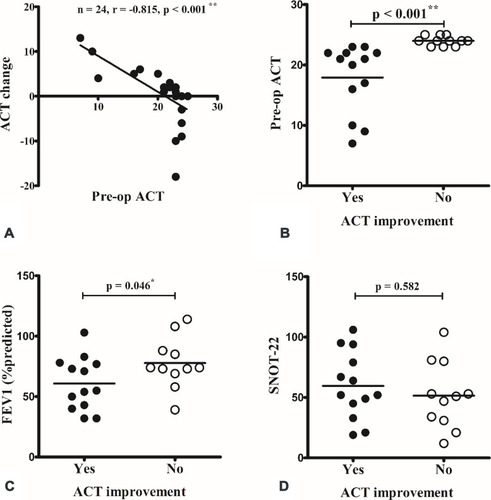
Figure 1 A strong correlation was observed between the Asthma Control Test (ACT) and Sino-Nasal Outcome Test-22 (SNOT-22) scores preoperatively (A) and 3 months postoperatively (B). ACT score was also well correlated with the predicted forced expiratory volume in 1 s (FEV1) (C), but not with total serum immunoglobulin (IgE) level (D). *p < 0.05; **p < 0.001 (Spearman correlation).
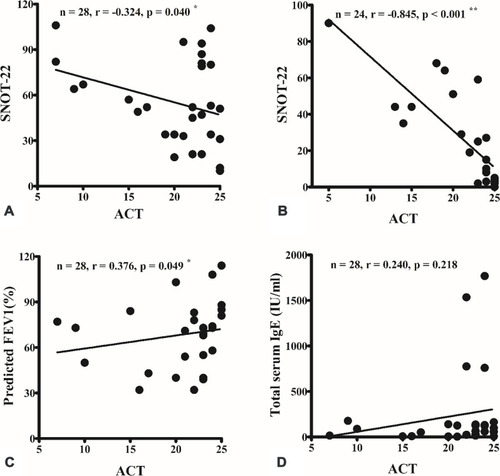
Figure 2 Nasal surgery improved sinonasal symptoms (A), but not asthma control (B) and the use of anti-asthma medication (C). The symbols represented patients with the same step of anti-asthma medication were overlapped. **p < 0.001 (Wilcoxon signed-rank test).

Figure 3 There was no significant difference between preoperative (pre-op) and postoperative (post-op) results of pulmonary function testing, including predicted forced vital capacity (FVC) (A), forced expiratory volume in 1 s (FEV1) (B) and FEV1/FVC (C).

Figure 4 The change in Asthma Control Test (ACT) scores were inversely correlated with the preoperative (pre-op) ACT score (A). When compared between patients with and without improvement in ACT after surgery, patients with postoperative ACT improvement had a worse pre-op ACT score (B) and predicted forced expiratory volume in 1 s (FEV1) (C). There was no difference in pre-op Sino-Nasal Outcome Test-22 (SNOT-22) score (D). *p < 0.05; **p < 0.001 (Spearman correlation and Mann–Whitney U-test).