Figures & data
Figure 1 Pathophysiology of OVA-induced asthma. OVA-induces different types of allergic asthma, including eosinophilic, neutrophilic, and mixed-granulocytic asthma. Although different sensitisation and challenge protocols has been used, the underlying mechanism is nearly similar. Dendritic cells (DCs) are the first innate immune cells encounters the allergen after crossing the respiratory epithelium. DCs process and present the antigen to the CD4+ T cells, which subsequently polarized into Th2 cells via Th2 inducing factor (IL-4). Th2 cells secrete copious amounts of cytokines (IL-4, IL-5, and IL-13), which later activate the naïve B cells to antigen-specific B cells (class switching). Further, antigen-specific B cells secret IgE, which sequentially recognized by the FcεRI on the mast cells and basophils. This process is called sensitisation. Upon re-exposure, allergen experienced leukocytes accelerate the priming process and activate mast cells and basophils. In addition, sensitized mast cells and basophils directly recognize the IgE antigen conjugates and undergo degranulation, which releases vasoactive amines (histamine), lipid mediators (prostaglandin, leukotrienes), chemokines, and other cytokines. As a net effect, the former mediators recruit the eosinophils and neutrophils, induce the mast cell differentiation, hypersecretion of mucus, Th1 cell activation, lung epithelial cells apoptosis, and others.Citation137 Of note, few protocols use LPS or Alum, which accelerate the process, to induce a specific type of allergic condition. The figure was created with the support of https://biorender.com under the paid subscription.
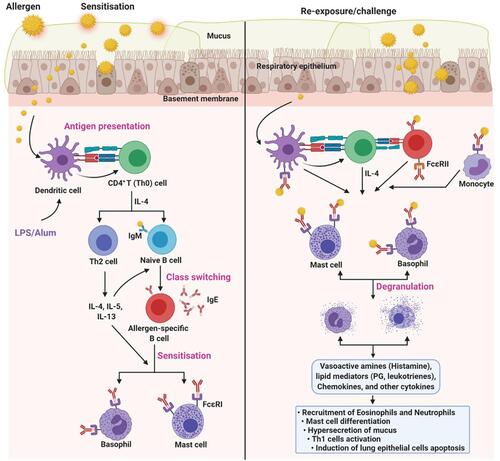
Table 1 Information About TMPs Conferring Protection Against OVA-Induced Asthma
Table 2 Study Protocol and the Protective Mechanism of TMPs Against OVA-Induced Asthma
Figure 2 Protocol followed to investigate TMPs against OVA-induced asthma. OVA-induced animal asthma model: (A) mice, (B) Guinea pig, (C) Rat. The above figure depicts the timeline of OVA sensitization and challenge followed by the end readouts. Schedules of sensitization and challenge depend on the type of animal model and routes of administration. In addition, varying OVA doses (with or without adjuvant) have been used both in sensitization and challenge (for more information, see ).
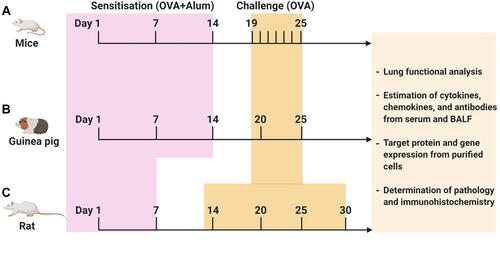
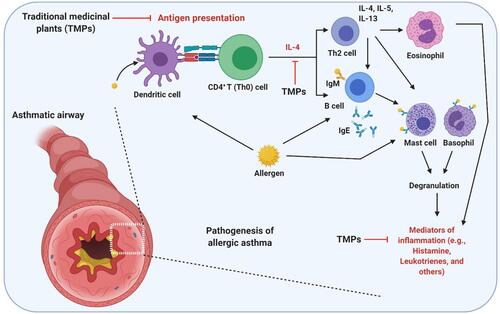
Figure 3 Possible mechanism of action of TMPs against OVA-induced asthma. As an allergen, OVA-induces airway inflammation and hyperresponsiveness. As a protein OVA recognized, processed and presented by the antigen-presenting cells. Upon presentation, CD4+ T helper (Th0) cells are activated and polarized toward Th2 phenotype, which activates eosinophils (Eosinophilic asthma), mast cells, and basophils to secret inflammatory mediators. OVA directly or indirectly (via Th cells mediated) activates the B lymphocytes to secret IgE, which is the main correlative factor in allergen-induced asthma. TMPs may either act by inhibiting antigen presentation or cytokine secretion or other inflammatory mediators (histamine, leukotrienes, and others). The figure was created with the support of https://biorender.com under the paid subscription.