Figures & data
Table 1 Types of Bronchial Epithelial Cells
Figure 1 Bronchial epithelial cells repertoire. Common cell types: basal cells, suprabasal cells, goblet cells, club cells (Clara cells) and ciliated cells. Rare cell types: neuroendocrine cells, ionocytes, Hillock cells and Tuft cells (brush cells). Created with affinity.serif.com.
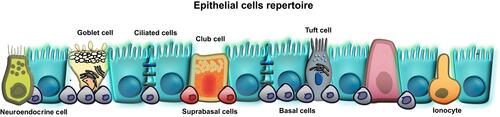
Figure 2 The junctional complex of bronchial epithelial cells. Tight junctions, adherens junction, gap junctions and desmosomes are intracellular junctions which regulate the transport of ions, water and macromolecules between tissue and lumen. TJs consist of claudins, occludin, tricellulin, and JAMs, located directly between neighboring bronchial epithelial cells. They directly interact with cytoplasmic TJs such as cingulin, MUPP1, MAGIs, non-PDZ proteins, and ZO-1, ZO-2, ZO-3 which bind directly to occludin and claudin on one end while also linking to actin fibers on the other end. Created with affinity.serif.com.
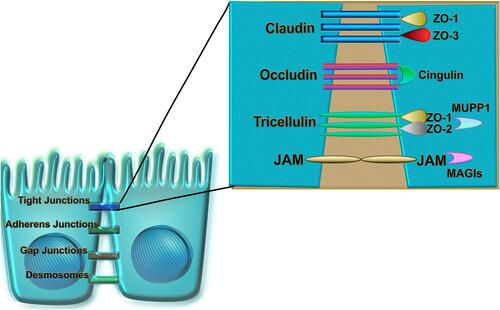
Figure 3 Mechanisms involved in a bronchial epithelial cell response to environmental factors and allergens. Airway epithelial cells are susceptible to damage as a result of exposure to allergens (house dust mite, pollen, and animal dander), pathogens (viruses, bacteria), and environmental toxins (air pollutants, cigarette smoke, ozone, detergents). Disruption of bronchial epithelium, indicated by red cell junctions, decreases the barrier integrity as evidenced by lower expression of TJs (occludin, ZO-1, E-cadherin, β-catenin, JAM and EGFR). Consequently, epithelial cells respond by secretion of cytokines IL-25, IL-33, and TSLP, which then attract other inflammatory cells like Th2 (IL-4, IL-5, IL-13), ILC2 (IL-13, IL-5), B cells, and dendritic cells (DC). Additional manifestations of respiratory disease occur in response to lipid mediators. Epithelial cells can also produce PAF and eicosanoids which have been shown to be chemotactic for neutrophils (neu), basophils (baso) and macrophages (mØ), activate eosinophils (eos) and macrophages, and alter vascular and epithelial permeability. Chronic inflammation also causes epigenetic changes in the bronchial epithelial cells by increasing DNA methylation and activating HDACs. Created with affinity.serif.com.
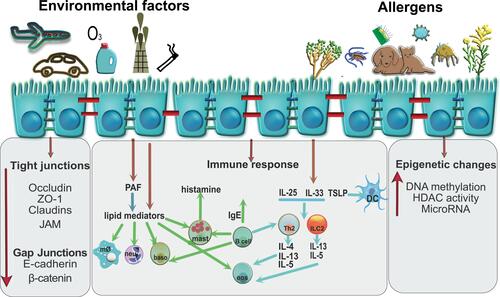
Table 2 Summary of Current and Novel Biological Therapies to Treat Asthma and Allergic Diseases
