Figures & data
Table 1 Characteristics and Ablation Parameter Data of 31 Patients with 35 Primary and Secondary Liver Cancers
Figure 1 A 50-year-old man had a 5.1 cm MLC lesion pathologically confirmed as gastric cancer. (A) CEUS showed a large-sized MLC nodule (51 × 47 mm) in segment VI/VII. (B) after extraction and storage of the 3D ultrasound volume image in the volume navigation system, the target MLC nodule (yellow) and its 5mm-AM (red) were outlined on 3DUS-US FI. (C and D) The target MLC nodules were ablated with two electrodes based on 3DUS-US FI guidance, particularly when the nodules became nonobvious after ablation. (E) After 12 ablation cycles, partial perfusion was observed within the nodules on 3DUS-CEUS FI (arrow). (F) Three immediate supplementary ablations were performed under 3DUS-US FI guidance. (G) 3DUS-CEUS FI was evaluated again and the non-perfusion area on the CEUS covered the entire target MLC nodule and its 5mm-AM. (H) One month later, contrast-enhanced CT confirmed the results of complete ablation.
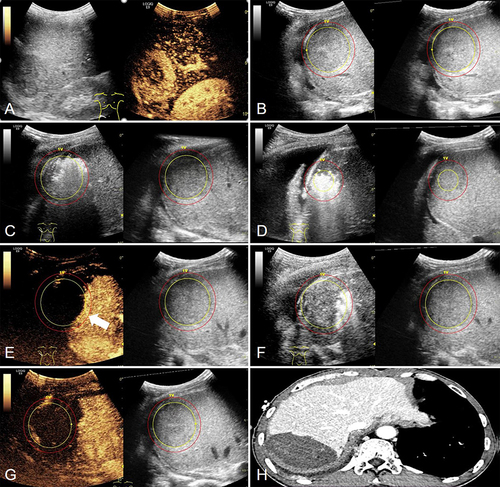
Figure 2 A 54-year-old woman had a 4.4 cm HCC lesion. (A) Contrast-enhanced MR showed a medium-sized HCC nodule (44 x 30 mm) in segment VI. (B) The DICOM format of contrast-enhanced MR was obtained and imported into the ultrasound FI system, and the target HCC nodules (yellow) and 5mm-AM (red) were outlined on the MR-US FI. (C and D) The target HCC nodules were ablated with a single electrode guided by MR-US FI, especially if the nodules became inconspicuous after ablation. (E) After 16 ablation cycles, MR-CEUS FI showed that the non-perfusion area on the CEUS covered the entire target HCC nodule and its 5mm-AM. (F) One month later, contrast-enhanced MR confirmed complete ablation.
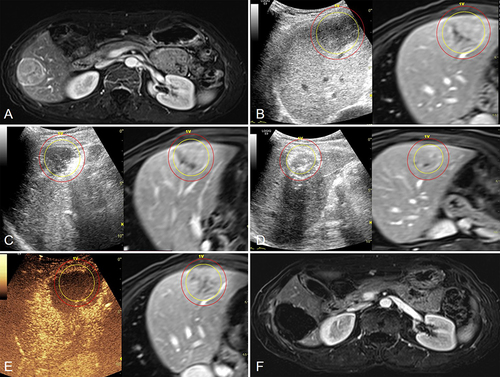
Table 2 Comparison of General Data, Ablation Parameters and Therapeutic Outcomes Between Medium-Sized and Large-Sized Groups
