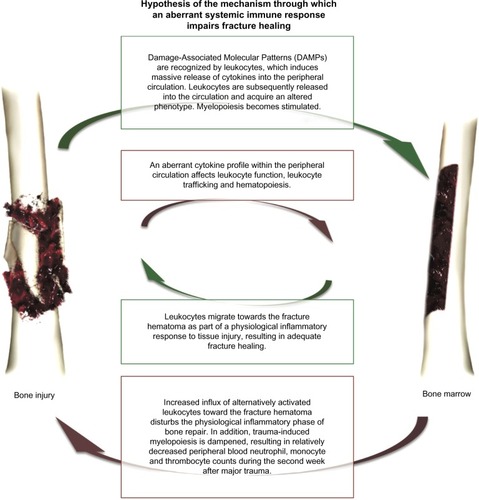
Figures & data
Figure 1 Peripheral blood counts of leukocytes (A), neutrophils (B), monocytes (C), and thrombocytes (D) during the first 2 weeks after major trauma.
Notes: Patients with normal (green) and impaired (red) fracture healing of the tibia. The peripheral blood-count curves of leukocytes, neutrophils, monocytes, and thrombocytes were analyzed with mixed linear models, and differed significantly between healing groups during the first 2 weeks after trauma (P-values were 0.0122, 0.0083, 0.0204, and <0.0001, respectively). In addition, each separate time point was compared between outcome groups using an independent t-test or nonparametric equivalent. For these subanalyses: *P<0.05; **P<0.01; ***P<0.001. Gray bars represent reference values.
Abbreviation: SEM, standard error of mean.
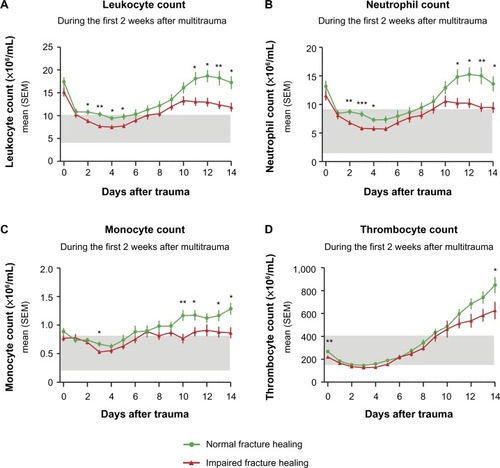
Figure 2 Peripheral blood lymphocyte counts (A), hemoglobin values (B) and the percentage of patients that required blood testing on each day (C) during the first two weeks after major trauma for patients with normal (green) and impaired (red) fracture healing of the tibia.
Notes: The peripheral blood lymphocyte counts and hemoglobin values were analyzed with mixed linear models, and these analyses showed no significant differences between the healing groups (P-values 0.0688 and 0.9275, respectively). In addition to the analyses with mixed linear models, each separate time point was also compared between outcome groups using an independent t-test or nonparametric equivalent. For these subanalyses: **P<0.01. Gray bars represent reference values.
Abbreviation: SEM, standard error of mean.
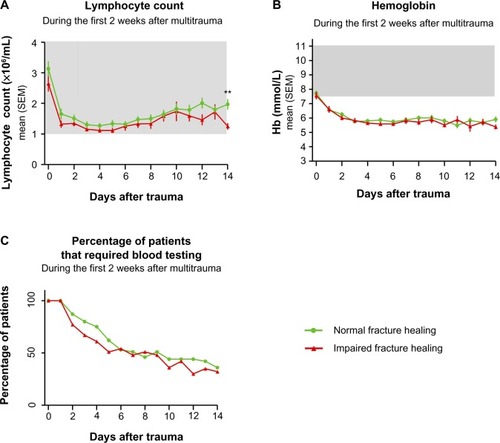
Table 1 Overview of clinical parameters of patients with normal and impaired fracture healing of the tibia