Figures & data
Figure 1 The pathogenesis of sepsis is characterized by both proinflammatory and anti-inflammatory mechanisms, and it is now believed that proinflammatory and anti-inflammatory can coexist, and that normally, proinflammatory and anti-inflammatory are in a dynamic equilibrium, which is disrupted by sepsis, which early on leads to the massive secretion of proinflammatory factors, reprogramming of the immune cells, and activation of the complement and coagulation systems, which further leads to a cytokine storm. Anti-inflammatory cytokines may be released subsequently or concurrently, and as the disease progresses, over-activation of the immune system leads to depletion of immune cells and sepsis progresses to an immunosuppressed state. The mechanisms of immunosuppression in sepsis and its complexity involve immune cell regulation, apoptosis autophagy, endotoxin tolerance, central nervous system, and metabolic changes. Therapies targeting immunosuppression in sepsis have the potential to be realized through these mechanisms.
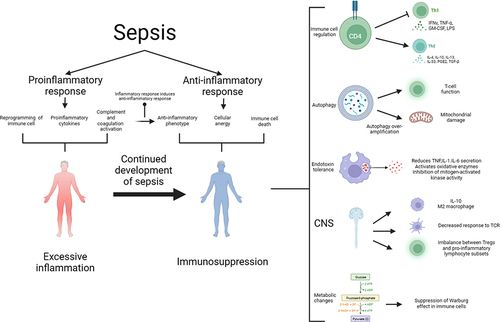
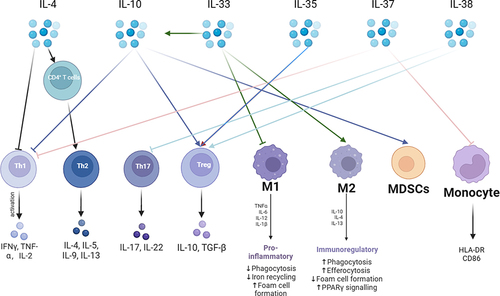
Figure 2 Anti-inflammatory cytokines are a very critical part of the immunosuppressive mechanism in sepsis. The mechanism of action of anti-inflammatory cytokines is very complex. The main anti-inflammatory cytokines are IL-4, IL-10, IL-33, IL-35, IL-37, and IL-38. IL-4 promotes the differentiation of CD4+ T lymphocytes into TH2 cells and releases anti-inflammatory cytokines. IL-10 can inhibit pro-inflammatory cytokine secretion and promote immunosuppressive cells Tregs with MDSCs. IL-33 promotes the immunosuppressive effects of IL-10 and promotes macrophage like M2 transformation. IL-35 promotes Tregs. IL-37 inhibits T lymphocyte and monocyte immune function. IL-38 inhibits TH17 and promotes Tregs.