Figures & data
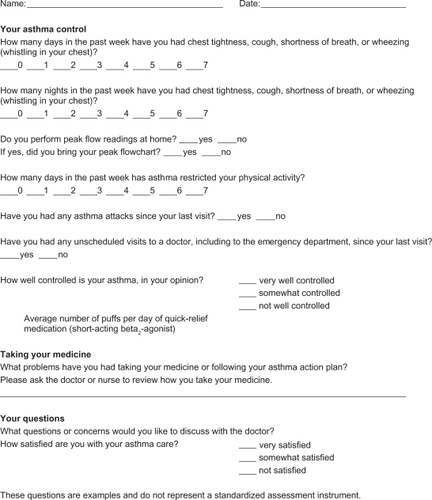
Figure 1 Methods of classifying asthma severity and initiating treatment in patients 12 years of age and older.
Abbreviations: EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICU, intensive care unit.
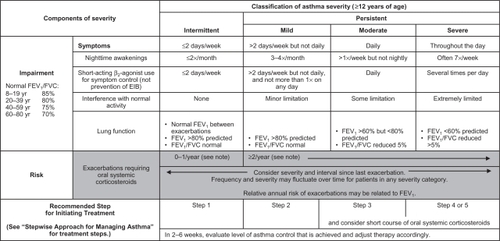
Figure 2 Methods of classifying asthma control and adjusting treatment in patients 12 years of age and older.
Abbreviations: FEV1, forced expiratory volume in 1 second; EIB, exercise-induced bronchospasm; N/A, not applicable; ATAQ, Asthma Therapy Assessment Questionnaire; ACQ, Asthma Control Questionnaire; ACT, Asthma Control Test.
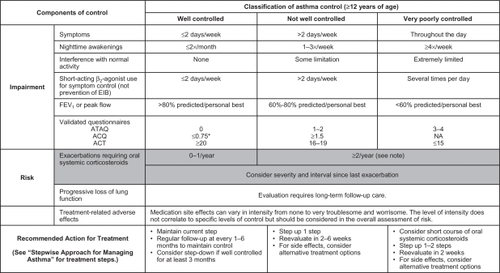
Figure 3 Stepwise approach for managing asthma in patients aged ≥12 years.
Abbreviations: ICS, inhaled corticosteroid; LABA, long-acting inhaled beta2-agonist; LTRA, leukotriene receptor antagonist; SABA, inhaled short-acting beta2-agonist.
Table 1 Classification of well-controlled asthma
Table 2 Validated instruments for assessing asthma controlCitation25–Citation27,Citation29
Figure 5 Overview of the allergic cascade. IgE (immunoglobulin E) is produced by the plasma cells, which are derived from B lymphocytes. The IgE moves through the extracellular fluid and vasculature until it binds to a high-affinity receptor, primarily found on mast cells and basophils. Cross-linking of the membrane IgE results in degranulation of the cell with mediator release and the resultant symptoms of asthma.
Ledford DK. Expert Opin Biol Ther. 2009;9:933–943. Copyright © 2009. Informa Healthcare. Reproduced with permission of Informa Healthcare.Citation49
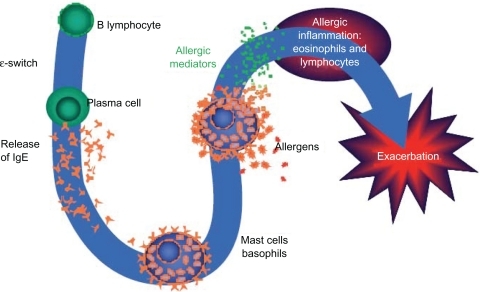
Table 3 Classes of asthma medicationsCitation7,Citation36–Citation38,Citation40
Table 4 Criteria for referring a patient with difficult-to-treat asthma to a specialist