Figures & data
Figure 1 Flowchart for the evaluation and diagnosis of chronic musculoskeletal pain at Hoshi General Hospital. First, orthopedic surgeons evaluate physical, neurological, and imaging findings and diagnose the presence of any specific musculoskeletal disorders. Second, physical therapists evaluate physical function. Third, psychiatrists diagnose any psychological disorders associated with chronic musculoskeletal pain, including psychiatric disorders. Fourth, clinical psychologists evaluate the psychosocial factors associated with pain. Finally, we perform brain magnetic resonance imaging and cerebral blood-flow scintigraphy to evaluate cortical function.
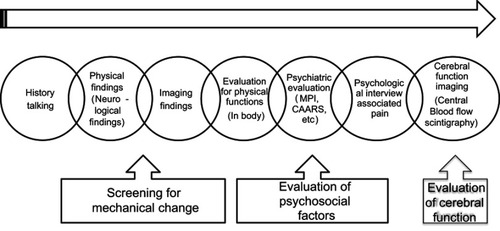
Figure 2 Changes in pain-associated factors. Statistically significant improvement was seen in: PCS (rumination) at 3 (p=0.03) and 6 (p=0.003) months after the program; PCS (helplessness) at 3 (p=0.012) and 6 (p=0.04) months; PDAS at 6 months (p=0.04); HADS (anxiety) at 6 months (p=0.016); and PSEQ immediately after (p=0.004), at 3 months (p=0.012), and at 6 months (p=0.03). *p<0.05.
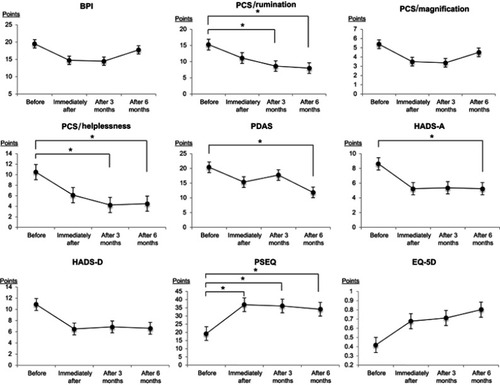
Figure 3 Changes in physical ability. Statistically significant improvement was seen in finger-floor distance (FFD) (flexibility) at 3 (p=0.04) and 6 (p=0.04) months after the program, and the 30-second sit-to-stand test (muscle endurance) at 6 months (p=0.012). *p<0.05.
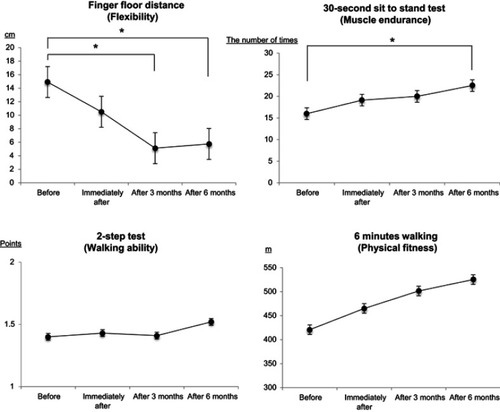
Table 1 Characteristics of the 23 cases
Table 2 Changes in pain and associated factors (n=23)
Table 3 Changes in physical functions (n=23)
Table 4 Outcomes at follow-up after inpatient programs in other countries
