Figures & data
Table 1 Sources of Risk of Bias and Cochrane Review Rating System
Table 2 Item Checklist for Assessment of Randomized Controlled Trials of IPM Techniques Utilizing IPM – QRB
Table 3 Qualitative Modified Approach to Grading of Evidence of Therapeutic Effectiveness Studies
Figure 1 Flow diagram illustrating the results of literature search conducted to evaluate lumbar radiofrequency thermoneurolysis.
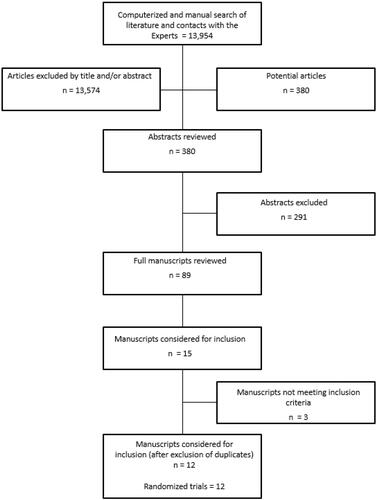
Table 4 Methodological Quality Assessment of Randomized Trials of Lumbar Facet Joint Radiofrequency Thermoneurolysis Utilizing Cochrane Review CriteriaCitation53
Table 5 Methodologic Quality Assessment of Randomized Trials of Lumbar Facet Joint Radiofrequency Thermoneurolysis Utilizing IPM – QRB CriteriaCitation54
Table 6 Study Characteristics of Randomized Controlled Trials Assessing Lumbar Radiofrequency Neurotomy
Table 7 Effectiveness of Lumbar Radiofrequency in Facet Joint Pain
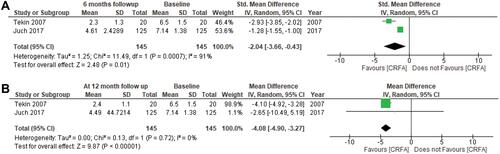
Figure 2 (A) Conventional dual-arm meta-analysis of pain relief of radiofrequency neurotomy vs sham control group at 6-month follow-up. (B) Conventional dual-arm meta-analysis of pain relief of radiofrequency neurotomy vs sham control group at 12-month follow-up.
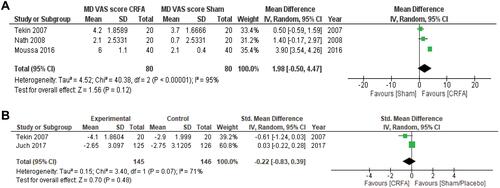
Figure 3 (A) Conventional dual-arm meta-analysis of pain relief of radiofrequency neurotomy of active control trials at 6 -month follow-up. (B) Conventional dual-arm meta-analysis of pain relief of radiofrequency neurotomy of active control trials at 12-month follow-up.
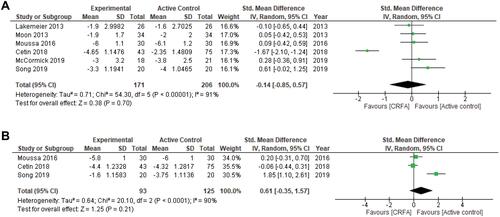
Figure 4 (A) Conventional dual-arm meta-analysis of functional status (ODI) of radiofrequency neurotomy vs sham control group at 6-month follow-up. (B) Conventional dual-arm meta-analysis of functional status (ODI) of radiofrequency neurotomy vs sham control group at 12-month follow-up.
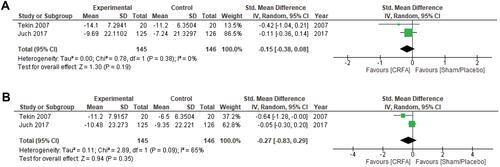
Figure 5 (A) Single arm meta-analysis of pain relief of radiofrequency neurotomy at baseline vs at 6-month follow-up of active-controlled trials. (B) Single arm meta-analysis of pain relief of radiofrequency neurotomy at baseline vs at 12-month follow-up of active control trials.
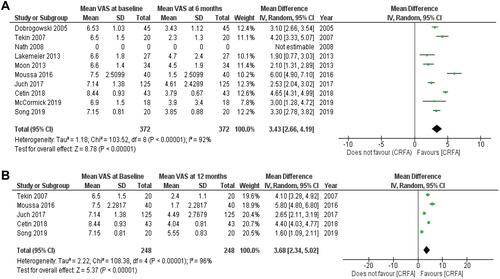
Figure 6 (A) Single-arm meta-analysis of functional status (ODI) of radiofrequency neurotomy at 6-month follow-up in sham control trials. (B) Single-arm meta-analysis of functional status (ODI) of radiofrequency neurotomy at 12 month follow-up in sham control trials.