Figures & data
Table 1 Demographics of sample
Figure 1 Familiarity and attitudes towards requirements proposed by the US Food and Drug Administration for ER/LA opioids. (A) Nearly a third of the primary care physicians in the sample (n = 201) reported that they were not familiar with REMS requirements proposed by the US Food and Drug for ER/LA opioids, rating familiarity as 1 or 2 on a 10-point scale. (B) Physicians vary widely on the effects of prescribing requirements on patient care (n = 201).
Abbreviations: FDA, Food and Drug Administration; ER/LA opioids, extended-release/long-acting opioids; REMS, Risk Evaluation and Mitigation Strategies.
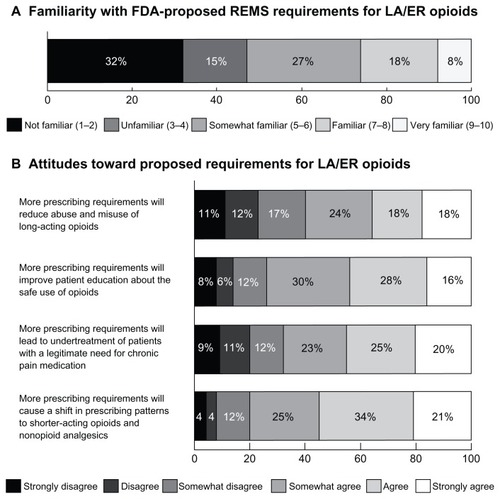
Table 2 Impact of potential components of opioid prescribing requirements on patient care (n = 201)
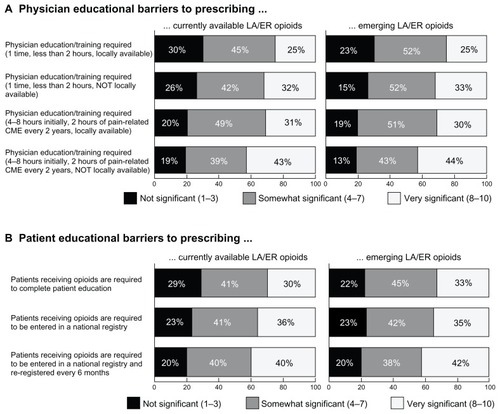
Figure 2 Physician and patient barriers to opioid prescription. (A) Respondents were asked to rate how significant certain potential requirements would be when prescribing currently available and emerging ER/LA opioids (n = 201). Locally available training and less time spent on mandatory education are factors seen as less burdensome to prescribing either set of opioids. Physicians also seem more likely to find training on currently available medications less burdensome than emerging therapies. (B) A third of surveyed primary care physicians (n = 201) would consider requiring patients receiving opioids to complete patient education to be a significant barrier to prescribing these therapies.
Abbreviation: ER/LA opioids, extended-release/long-acting opioids; CME, continuing medical education.